Leadership in Healthcare
Comprehensive Notes for Nursing Students
Introduction
Effective healthcare leadership is crucial for delivering quality patient care, managing healthcare teams, and addressing community health needs. These notes explore various leadership approaches, community health management strategies, and practical methods for organizing health camps and village clinics.
Table of Contents
Leadership Approaches in Healthcare Settings
Healthcare leaders must adopt appropriate leadership styles based on their team composition, organizational goals, and specific healthcare settings. Research indicates that effective healthcare leadership often involves a combination of adaptive, situational, transformational, and ethical leadership styles that create a resilient and responsive healthcare environment.
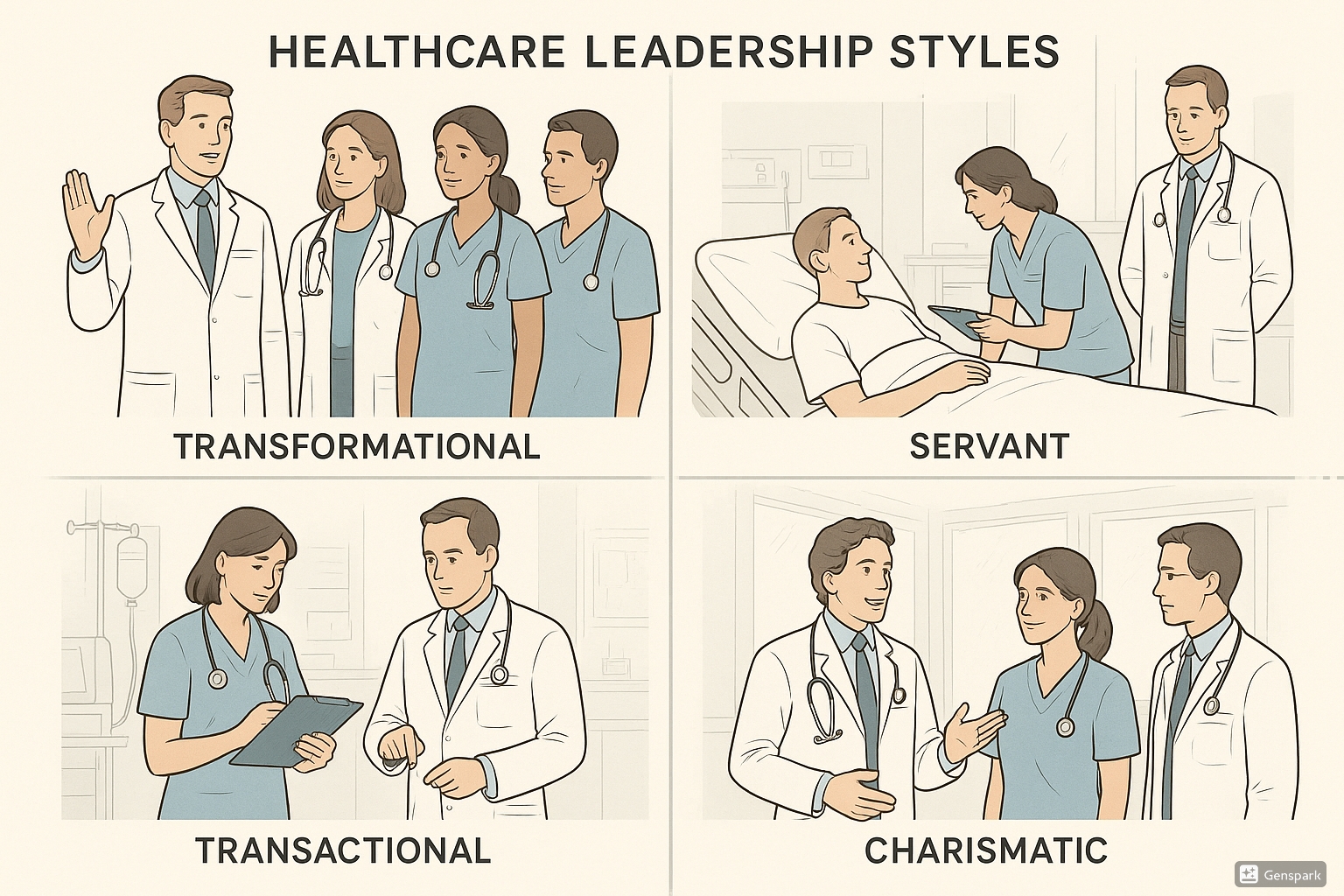
Transformational Leadership
Focuses on innovation, problem-solving, and future planning. Leaders inspire and motivate team members to exceed expectations.
- Encourages innovation and is tolerant of errors
- Focuses on practical aspects and new approaches
- Best for healthcare systems requiring substantial changes
- Improvement effectiveness: 14% in before-after studies
Servant Leadership
Leaders prioritize supporting team members’ development and skill building while involving them in organizational goals.
- Creates a sharing leadership environment
- Provides steady support for team members
- Emphasizes collaboration and empowerment
- One of the most implemented styles in healthcare (42.9% in studies)
Charismatic (Emotive) Leadership
Based on strong emotional connections between leader and team. Leaders use their charisma to inspire motivation and commitment.
- Improves worker motivation through emotional connection
- Uses leader’s foresight and planning strategies
- Particularly effective in smaller healthcare units
- Second most common style (38.1% in studies)
Transactional Leadership
Focuses on structure, clear expectations, rewards, and technical aspects of healthcare delivery.
- Emphasizes technical skills and structured protocols
- Creates two-way knowledge sharing processes
- Utilizes reward systems for performance
- More effective in private hospitals and South American contexts
- Transformational – Transforms the healthcare system through innovation
- Charismatic – Connects emotionally with team members
- Servant – Serves team members by supporting their growth
- Transactional – Trades performance for rewards in a structured system
Leadership Style Effectiveness by Setting
| Setting/Context | Most Effective Style | Key Benefits |
|---|---|---|
| Systems requiring major change | Transformational | Innovation, vision, overcoming resistance |
| Private hospitals | Transactional | Cost-effectiveness, performance metrics, rewards |
| Medical specialties | Servant/Charismatic | Team cohesion, skill development, emotional support |
| Surgical settings | Mixed (challenging context) | Requires situational adaptation due to high pressure |
| Multi-professional teams | Servant | Collaboration across disciplines, skill sharing |
Taking Control of Community Health
Community health leadership involves mobilizing resources, engaging stakeholders, and implementing strategic initiatives to improve health outcomes at the population level.
Community Health Leadership Framework
Effective community health leadership requires a comprehensive approach that addresses social determinants of health while engaging key stakeholders in creating sustainable solutions.
Key Components
- Community needs assessment
- Stakeholder engagement
- Resource mobilization
- Educational initiatives
- Data-driven decision making
- Sustainability planning
Essential Skills
- Cultural competence
- Communication across barriers
- Ethical leadership
- Partnership development
- Resource allocation
- Health promotion
Community Health Leadership Strategies
1. Community Engagement Model
Building relationships with community leaders, organizations, and residents is essential for successful community health initiatives. This approach recognizes that local knowledge and engagement are critical for sustainability.
- Enlisting community leaders as champions
- Needs assessment through participatory methods
- Generating shared vision for health improvement
- Aligning resources with community priorities
- Governing together through inclusive structures
- Evaluating outcomes collaboratively
2. Health Equity Approach
Addressing disparities in health outcomes requires targeted strategies that recognize and address the social determinants of health affecting vulnerable populations.
Assessment
Identifying health disparities through data analysis and community input
Intervention
Implementing tailored programs addressing specific barriers to care
Sustainability
Building capacity within communities to maintain health improvements
3. Multi-sector Partnerships
Creating alliances across sectors (healthcare, education, housing, transportation) to address complex health challenges that no single entity can solve alone.
Partnership Development Steps:
- Identify and engage key stakeholders across sectors
- Establish shared vision and goals for community health
- Develop structured governance and communication frameworks
- Share resources and align efforts for maximum impact
- Track shared metrics and outcomes for collective accountability
Organizing Health Camps
Health camps are strategic interventions where healthcare professionals “camp” in an underserved area to provide concentrated healthcare services, screenings, and education. Effective organization of health camps requires careful planning, community engagement, and structured implementation.
10-Point Checklist for Organizing Health Camps
Follow this evidence-based checklist to ensure your health camp is meaningful and effective:
Define specific, measurable goals for the health camp (e.g., screening for specific conditions, providing vaccinations, health education).
Conduct thorough assessment of local health needs through surveys, interviews, and existing health data.
Review lessons from any previous health camps in the area and address identified gaps or challenges.
Ensure connection with a supporting hospital or healthcare organization for referrals and follow-up care.
Engage local healthcare workers, facilities, and health authorities in planning and implementation.
Define specific roles for all stakeholders including medical staff, volunteers, community members, and administrative support.
Map and mobilize necessary resources including human resources, medications, equipment, funding, and infrastructure.
Secure necessary permissions, documentation, and logistical support from relevant authorities.
Develop methods to assess camp effectiveness, including metrics for services delivered, patients served, and outcomes achieved.
Create structured approach for addressing key findings and continuing care after the camp concludes.
Key Domains for Health Camp Organization
| Domain | Activities |
|---|---|
| Resource Mobilization |
|
| Information, Education & Communication |
|
| Community Participation |
|
| Clinical Care |
|
| Event Management |
|
- Community engagement & needs assessment
- Align resources with objectives
- Mobilize multidisciplinary teams
- Plan logistics and clinical protocols
- Sustainability through follow-up systems
Village Clinics Implementation
Village clinics provide sustainable healthcare access in rural and underserved communities. Implementing effective village clinics requires understanding local contexts, building appropriate infrastructure, and ensuring continuity of care.
Village Clinic Models
Fixed Village Clinics
Permanent healthcare facilities established within villages to provide routine care.
Key Components:
- Permanent physical structure
- Basic diagnostic capabilities
- Essential medication supplies
- Trained local healthcare workers
- Referral pathways to higher facilities
Mobile Village Clinics
Rotating healthcare services that visit multiple villages on a scheduled basis.
Key Components:
- Transportation for healthcare team
- Portable diagnostic equipment
- Scheduled visitation calendar
- Local coordination points
- Mobile health records system
Challenges in Rural Healthcare Settings
Rural communities face significant barriers to healthcare access that village clinics must address:
- Limited availability of healthcare professionals (80% of doctors are in urban areas)
- Geographic isolation with travel distances up to 100km for healthcare
- Infrastructure constraints (power, water, roads)
- Limited diagnostic and treatment capabilities
- Higher prevalence of preventable diseases
- Financial barriers to seeking care
Implementation Framework for Village Clinics
1. Community Assessment and Engagement
- Conduct healthcare needs assessment
- Map existing healthcare resources and gaps
- Engage community leaders and stakeholders
- Build consensus on clinic model and priorities
2. Resource Planning
- Identify funding sources and sustainability models
- Recruit and train healthcare providers (consider local training models)
- Establish infrastructure requirements
- Create supply chain for medications and consumables
3. Service Delivery Model
- Define scope of services based on community needs
- Develop clinical protocols adapted for limited resources
- Create referral pathways to secondary and tertiary care
- Implement health information systems
4. Technology Integration
- Deploy appropriate telehealth solutions
- Implement mobile health records systems
- Utilize point-of-care diagnostics
- Consider digital health education platforms
5. Monitoring and Evaluation
- Establish key performance indicators
- Implement quality improvement processes
- Collect and analyze service utilization data
- Measure health outcomes and community satisfaction
- Resource optimization in limited settings
- Understanding community needs and preferences
- Referral systems for comprehensive care
- Appropriate technology integration
- Local capacity building and sustainability
Best Practices & Updates in Healthcare Leadership
1. Adaptive Leadership in Crisis Response
Recent experiences in global health crises have demonstrated the value of adaptive leadership approaches that can rapidly respond to changing conditions. Healthcare leaders should develop crisis response frameworks that balance structured protocols with flexibility and innovation.
2. Digital Health Integration in Rural Settings
Emerging technologies are transforming healthcare delivery in resource-limited settings. Healthcare leaders should strategically implement digital health solutions such as telehealth, mobile health applications, and cloud-based electronic health records while addressing challenges related to connectivity, digital literacy, and data security.
3. Collaborative Multi-Sector Partnerships
Addressing complex health challenges requires collaboration across sectors. Healthcare leaders should develop skills in building and managing partnerships with government agencies, NGOs, educational institutions, and private sector organizations to leverage diverse resources and expertise for community health improvement.
Conclusion
Effective healthcare leadership is multifaceted, requiring adaptation of leadership styles to specific contexts while addressing the unique challenges of community health management. By implementing evidence-based approaches to organizing health camps and village clinics, healthcare leaders can significantly improve healthcare access and outcomes in underserved communities.
The integration of appropriate leadership styles, community engagement strategies, and structured implementation frameworks provides a comprehensive approach to addressing healthcare challenges at both organizational and community levels.
