Shared Care & Electronic Health Records: Standards and Challenges
Comprehensive educational resource for nursing students
Table of Contents
- 1. Introduction to Electronic Health Records
- 2. Shared Care Records: Concept & Implementation
- 2.1 Benefits of Shared Care Records
- 2.2 Implementation Challenges
- 3. Challenges of Capturing Rich Patient Histories
- 3.1 Data Standardization & Integration
- 3.2 Managing Unstructured Data
- 3.3 Privacy & Security Concerns
- 4. Global Developments in EHR Standards
- 4.1 FHIR: The Next Generation Standard
- 4.2 Different Country Approaches
- 4.3 Future Trends in EHR Systems
- 5. Interoperability: The Key to Successful EHR Integration
- 5.1 Levels of Interoperability
- 5.2 Challenges & Solutions
- 6. The Role of Nurses in EHR Implementation
- 7. Mnemonics & Learning Aids for EHR Systems
- 8. Case Studies & Real-world Applications
- 9. Summary & Key Takeaways
- 10. References & Additional Resources
1. Introduction to Electronic Health Records
Electronic Health Records (EHRs) represent a significant advancement in healthcare information management, transforming how patient data is collected, stored, accessed, and shared across healthcare systems. Unlike traditional paper records, EHRs provide a comprehensive, digital version of a patient’s medical history, enabling healthcare providers to make more informed decisions and deliver more coordinated care.
Definition & Core Components
An Electronic Health Record (EHR) is an electronic version of a patient’s medical history maintained by healthcare providers over time, including demographics, progress notes, medications, vital signs, past medical history, immunizations, laboratory data, and radiology reports.
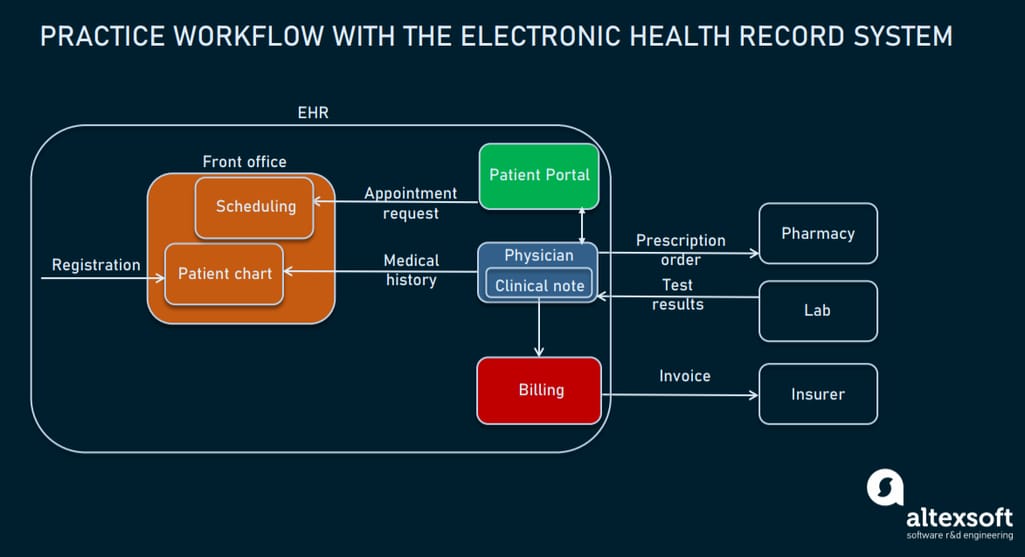
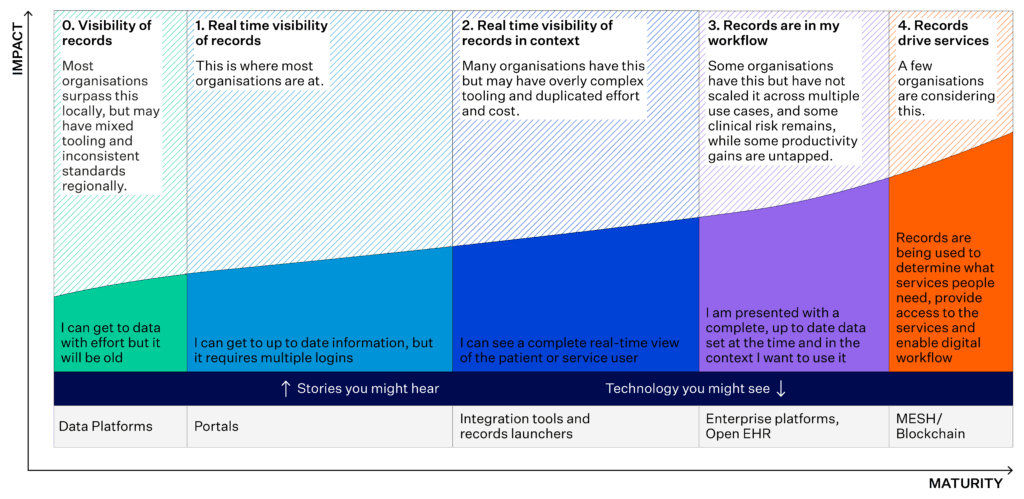
Fig 1: Components of an Electronic Health Record System
Evolution of Electronic Health Records
Early computerized systems developed by academic medical centers and government agencies. These systems focused primarily on administrative tasks rather than clinical applications.
Development of more sophisticated systems with clinical capabilities. The Institute of Medicine published reports on improving health record systems.
Shift toward comprehensive electronic health records with integration capabilities. Introduction of the HITECH Act in 2009, which provided incentives for healthcare providers to adopt EHR systems.
Focus on interoperability between different EHR systems. Development of standards like HL7 and FHIR to enable data exchange.
Integration of artificial intelligence, machine learning, and advanced analytics with EHRs. Enhanced patient access and control over their health data. Continued emphasis on interoperability and shared care models.
Benefits of EHR Systems
- Improved Patient Care: Provides real-time, comprehensive patient information at the point of care
- Enhanced Coordination: Facilitates communication between healthcare providers across different settings
- Reduced Errors: Decreases medication errors and adverse drug events through automated checks
- Better Accessibility: Enables remote access to patient records, supporting telehealth initiatives
- Improved Decision Making: Provides clinical decision support tools based on patient data
- Enhanced Efficiency: Reduces administrative burden through automated workflows
- Data Analytics: Supports population health management and research through aggregated data
- Interoperability: When properly implemented, allows for seamless information exchange between systems
Critical Considerations
While EHR systems offer numerous benefits, they also present challenges related to implementation costs, workflow disruptions, user training, data security, and interoperability issues. Understanding these challenges is crucial for successful adoption and utilization.
3. Challenges of Capturing Rich Patient Histories in a Computable Form
Converting comprehensive patient histories into a structured, computable format represents one of the most significant challenges in modern healthcare informatics. While traditional paper records allowed for narrative flexibility, electronic systems require more structured data to enable searching, analysis, and interoperability.
3.1 Data Standardization & Integration
Patient histories include complex, multidimensional information that can be difficult to standardize:
Components of a Rich Patient History
- Chief complaints and presenting symptoms
- Past medical history from various care settings
- Surgical history with complications
- Medication history including over-the-counter drugs
- Allergies and reactions
- Family health history across generations
- Social history including lifestyle factors
- Mental health history
- Occupational exposures and risks
- Cultural factors affecting health
The process of standardizing this diverse information presents several challenges:
Terminology Variations
Different providers may use varied terms for the same condition (e.g., “heart attack” vs. “myocardial infarction”), requiring standardized medical terminologies like SNOMED CT or ICD-10.
Granularity Issues
Systems need to capture both broad categories and specific details, balancing structured data with clinical nuance and contextual information.
Legacy Data Integration
Converting historical paper records and integrating data from older electronic systems with varying formats presents significant standardization challenges.
3.2 Managing Unstructured Data
Patient narratives often contain rich contextual information that doesn’t fit neatly into structured fields:
The Unstructured Data Challenge
Studies estimate that 80% of healthcare data is unstructured, including clinical notes, patient descriptions of symptoms, and contextual information about health experiences. This unstructured data often contains critical insights that can be lost when forced into rigid templates.
Approaches to Managing Unstructured Data
- Natural Language Processing (NLP): Technologies that can extract meaning from free text and convert it into structured data
- Hybrid Documentation Models: Systems that combine structured data entry with free-text fields
- Semantic Tagging: Adding metadata to narrative text to enable searching and analysis
- Voice Recognition: Converting spoken narratives into searchable text
- AI-Assisted Documentation: Systems that suggest structured codes based on narrative descriptions
Example: Structured vs. Unstructured Data
Structured Form:
Diagnosis: Type 2 Diabetes Mellitus (E11.9)
Onset Date: 01/15/2020
Medications: Metformin 500mg, twice daily
Unstructured Narrative:
“Patient reports difficulty controlling blood sugar despite diet modifications. They mentioned occasional dizziness when skipping meals and are concerned about recent weight loss despite increased appetite. Family history significant for diabetes in mother and maternal grandfather.”
The narrative contains important contextual information about symptoms, concerns, and family history that may not be fully captured in structured fields.
3.3 Privacy & Security Concerns
Capturing comprehensive patient histories raises important privacy and security considerations:
| Concern | Challenge | Potential Solution |
|---|---|---|
| Sensitive Information | Histories may contain highly sensitive information (mental health, substance use, STIs) | Granular consent models allowing patients to control access to different types of information |
| Data Sharing | Balancing comprehensive data sharing with patient privacy | Role-based access controls and audit trails |
| Family Information | Patient histories often contain health information about relatives | De-identification of family members while preserving clinical relevance |
| Secondary Use | Using patient history data for research or population health | Transparent consent processes and anonymization techniques |
| Data Security | Protecting comprehensive histories from breaches | Encryption, secure authentication, and regular security audits |
Emerging Solutions
Recent advances are helping address these challenges:
- Structured Clinical Documentation Support: Tools that guide clinicians through systematic history-taking while reducing documentation burden
- Patient-Generated Health Data: Systems allowing patients to contribute to their own histories through portals and apps
- Advanced Analytics: AI systems that can identify patterns and connections across complex patient histories
- Blockchain Technology: Providing secure, verifiable history records with patient-controlled access
4. Global Developments in EHR Standards
The landscape of Electronic Health Record standards continues to evolve globally, with different countries and regions adopting varied approaches to implementation and standardization. Understanding these international developments is crucial for nursing professionals working in increasingly global healthcare environments.
4.1 FHIR: The Next Generation Standard

Fig 3: FHIR Standard Framework – Fast Healthcare Interoperability Resources
Fast Healthcare Interoperability Resources (FHIR) has emerged as a transformative standard for health data exchange, addressing many limitations of previous standards and driving global interoperability efforts:
Key Features of FHIR
- RESTful API architecture familiar to modern web developers
- Resources-based model with discrete, reusable components
- Human-readable formats (JSON, XML) alongside machine-readable encoding
- Extension capability allowing customization while maintaining interoperability
- Implementation focus with practical tools and libraries
- Open standard with free specifications and reference implementations
- Robust community of developers and healthcare organizations
- Version compatibility ensuring smoother transitions between releases
FHIR vs. Traditional Standards
Unlike previous standards like HL7 v2 or v3, FHIR combines the best features of these approaches with modern web technologies. It enables granular data access (retrieving specific information rather than entire documents) and supports both document-based and message-based exchange paradigms.
4.2 Different Country Approaches
EHR adoption and standardization vary significantly across countries, influenced by healthcare systems, regulatory frameworks, and cultural factors:
| Country/Region | EHR Approach | Key Features | Standards Adopted |
|---|---|---|---|
| United States | Market-driven with regulatory incentives | Fragmented implementation; emphasis on meaningful use and interoperability | HL7, FHIR, SNOMED CT, LOINC |
| European Union | Federated approach with cross-border exchange | eHealth Digital Service Infrastructure; emphasis on cross-border care | epSOS, ISO/EN 13606, HL7 FHIR |
| United Kingdom | Centralized national system with regional variations | NHS Digital transformation; Summary Care Records | SNOMED CT, dm+d, FHIR UK Core |
| Estonia | Nationwide integrated system | X-Road infrastructure; patient-owned data with blockchain security | HL7 CDA, DICOM, LOINC |
| Australia | National system with opt-in model | My Health Record; focus on patient control | FHIR AU, SNOMED CT-AU, AMT |
| Japan | Regional networks with national standardization | SS-MIX2 standardized storage; emphasis on disaster preparedness | HL7 v2.5, SS-MIX, JLAC |
Commonalities in Global Approaches
- Movement toward patient-centered models
- Recognition of interoperability as a critical priority
- Integration of mobile health and telehealth
- Increasing focus on cybersecurity
- Growing adoption of international standards
Key Differences
- Centralized vs. decentralized approaches
- Mandatory vs. voluntary adoption models
- Government-driven vs. private sector-led development
- Varying approaches to patient consent and control
- Different priorities in functionality and use cases
4.3 Future Trends in EHR Systems
The continuing evolution of EHR systems is being shaped by several emerging trends and technologies:
AI and Machine Learning
- Predictive analytics for patient risk
- Natural language processing for documentation
- Clinical decision support enhancements
- Automated coding and billing
Patient-Generated Health Data
- Integration of wearable device data
- Patient-reported outcomes
- Home monitoring capabilities
- Mobile health application connectivity
Cloud-Based EHR Solutions
- Improved accessibility and scalability
- Reduced infrastructure costs
- Enhanced disaster recovery
- Easier updates and maintenance
Advanced Security Measures
- Blockchain for data integrity
- Biometric authentication
- Zero trust security frameworks
- Federated identity management
Enhanced Interoperability
- FHIR API adoption acceleration
- Cross-border data exchange
- Standardized terminologies
- API-first design approaches
User Experience Focus
- Voice-enabled documentation
- Contextual user interfaces
- Workflow optimization
- Reduced cognitive burden
Implementation Challenges Remain
Despite these advances, significant challenges persist in global EHR implementation, including variable infrastructure in low-resource settings, differences in privacy regulations, workforce training needs, and concerns about data ownership and control. Healthcare organizations and governments must address these challenges while pursuing the benefits of sophisticated EHR systems.
5. Interoperability: The Key to Successful EHR Integration
Interoperability refers to the ability of different information systems, devices, and applications to access, exchange, integrate, and cooperatively use data in a coordinated manner within and across organizational boundaries. In healthcare, interoperability is essential for ensuring that patient data can flow seamlessly between different systems and care settings.

Fig 4: FHIR Enabling Interoperability Between Healthcare Systems
5.1 Levels of Interoperability
Interoperability in healthcare exists on several distinct levels, each building upon the previous one:
1. Foundational Interoperability
Enables data exchange from one system to another without requiring the receiving system to interpret the data. This basic level ensures that data can be received but doesn’t guarantee meaningful use.
Example: A laboratory system sending raw test results to an EHR without any specification of what the data means or how it should be used.
2. Structural Interoperability
Defines the format, syntax, and organization of data exchange. This intermediate level ensures that the clinical or operational purpose and meaning of data are preserved and unaltered.
Example: Systems using standardized message formats (like HL7) to exchange information, where the receiving system can identify specific data fields like patient name or diagnosis code.
3. Semantic Interoperability
Enables different systems to interpret and effectively use the exchanged information. This advanced level requires standardized terminologies and ontologies to ensure consistent understanding across systems.
Example: Two different EHR systems exchanging a diagnosis coded in SNOMED CT, with both systems able to understand the clinical meaning and implications of the diagnosis.
4. Organizational Interoperability
Encompasses broader governance, policy, legal, social, and organizational aspects that facilitate seamless collaboration and communication between different systems and organizations.
Example: Healthcare networks with coordinated workflows, where a primary care order placed in one system triggers appropriate actions and notifications in specialist and pharmacy systems.
5.2 Interoperability Challenges & Solutions
Despite significant progress, healthcare organizations continue to face substantial challenges in achieving true interoperability:
| Challenge | Description | Potential Solutions |
|---|---|---|
| Technical Heterogeneity | Different systems using varied technologies, data models, and architectures | Adoption of open standards like FHIR; implementation of API-first approaches; middleware solutions |
| Data Standardization | Inconsistent terminologies, codes, and data structures | Implementation of standard clinical terminologies (SNOMED CT, LOINC); data mapping and translation services |
| Information Blocking | Intentional or unintentional practices that interfere with data sharing | Regulatory requirements (21st Century Cures Act); incentives for data sharing; collaboration frameworks |
| Privacy and Security | Concerns about unauthorized access during data exchange | Granular consent management; secure authentication protocols; encryption; audit trails |
| Legacy Systems | Older systems without modern interoperability capabilities | Integration engines; API gateways; progressive modernization strategies |
| Workflow Integration | Technical interoperability without clinical workflow integration | User-centered design; workflow analysis; clinical decision support integration |
| Cost and Resources | Financial and expertise barriers to implementing interoperability solutions | Cloud-based solutions; shared services; government incentives; open-source implementations |
Success Factors for Interoperability Initiatives
- Stakeholder Engagement: Involving clinicians, administrators, IT staff, and patients in planning and implementation
- Clear Governance: Establishing policies, responsibilities, and decision-making processes for data sharing
- Standards Adoption: Committing to recognized international and national standards
- Incremental Approach: Starting with targeted use cases and expanding gradually
- Continuous Testing: Regular validation of interoperability capabilities through testing and certification
- Ongoing Training: Ensuring staff understand how to effectively use interoperable systems
6. The Role of Nurses in EHR Implementation
Nurses play a pivotal role in the successful implementation and utilization of Electronic Health Record systems. As the healthcare professionals who spend the most time with patients and document significant portions of patient care, nurses are essential stakeholders in EHR design, implementation, and optimization.
Key Nursing Responsibilities in EHR Systems
- Clinical Documentation: Recording patient assessments, interventions, responses, and outcomes
- Medication Administration: Documenting medication administration and monitoring effects
- Care Planning: Creating and updating nursing care plans in electronic format
- Patient Education: Documenting education provided and patient understanding
- Communication: Facilitating interdisciplinary communication through EHR tools
- Clinical Decision Support: Using and providing feedback on decision support features
- Quality Improvement: Participating in data collection and analysis for quality initiatives
Nurse Involvement in EHR Projects
For successful EHR implementation, nurses should be involved in:
System Selection and Design
Providing input on nursing workflows and documentation needs
Configuration and Customization
Helping to design templates and workflows that reflect nursing practice
Testing and Validation
Participating in usability testing and clinical validation
Training and Support
Serving as super-users and trainers for nursing colleagues
Continuous Improvement
Participating in optimization efforts and providing ongoing feedback
EHR Implementation Challenges for Nurses
- Increased Documentation Time: EHR systems can initially increase time spent on documentation
- Workflow Disruptions: Changes to established workflow patterns require adaptation
- Technology Anxiety: Varying comfort levels with technology among nursing staff
- Alert Fatigue: Excessive notifications can lead to important alerts being overlooked
- Focus on Computers vs. Patients: Concern about reduced direct patient interaction
Best Practices for Nursing Documentation in EHRs
Documentation Principles
- Use objective, factual language
- Document in real-time when possible
- Be comprehensive but concise
- Include patient quotes when relevant
- Follow institutional documentation policies
- Use standardized terminology
Avoiding Common Errors
- Avoid copy-paste without verification
- Don’t use unapproved abbreviations
- Prevent incorrect auto-completions
- Document in the correct patient record
- Ensure timely documentation
- Avoid inappropriate workarounds
Efficiency Strategies
- Learn keyboard shortcuts
- Use approved templates appropriately
- Document progressively throughout shift
- Use mobile documentation devices
- Master search functionalities
- Organize information logically
Nursing Informatics: A Growing Specialty
Nurse informaticists play a crucial role in bridging clinical nursing practice and information technology. They help design EHR systems that support nursing practice, develop clinical decision support tools, conduct usability testing, and lead implementation projects. As EHR systems become increasingly sophisticated, demand for nurses with informatics expertise continues to grow.
Future Directions: Nursing and Advanced EHR Features
As EHR systems evolve, nurses will increasingly engage with advanced features such as:
- AI-assisted documentation that can draft notes from audio recordings
- Predictive analytics that alert nurses to potential patient deterioration
- Integration with IoT devices for automated vital signs and assessments
- Virtual nursing assistants that can handle routine documentation tasks
- Enhanced visualization tools for complex patient data
7. Mnemonics & Learning Aids for EHR Systems
Memory aids and mnemonics can be valuable tools for nursing students learning to navigate and document in Electronic Health Record systems. These devices help organize information and ensure comprehensive documentation while reducing cognitive load.
“CHART” for EHR Documentation
-
C
Clear and Concise
Document facts objectively, avoiding redundant information
-
H
Holistic Documentation
Include physical, psychological, social, and spiritual aspects of care
-
A
Accurate Terminology
Use standardized terms and avoid unapproved abbreviations
-
R
Real-time Recording
Document as soon as possible after care to ensure accuracy
-
T
Thorough Reviews
Check documentation for completeness and accuracy before finalizing
“FAIR” for Interoperability Awareness
-
F
Format Correctly
Use standardized formats and structured fields when available
-
A
Avoid Free Text for Key Data
Use structured fields for data that needs to be shared between systems
-
I
Include Required Elements
Ensure all required fields are completed for proper data exchange
-
R
Recognize Shared Information
Be aware of which information will be shared with other systems or providers
“SECURE” for EHR Privacy & Security
-
S
Sign Out Every Time
Always log out when finished with the EHR
-
E
Ensure Screen Privacy
Position screens away from public view and use privacy screens
-
C
Credentials Are Private
Never share passwords or login information
-
U
Use Only Authorized Access
Access only records needed for your direct patient care
-
R
Report Security Incidents
Immediately report any potential breaches or concerns
-
E
Educate Yourself on Policies
Stay current on organizational privacy policies and procedures
“PATIENT” for Capturing Patient History
-
P
Present Illness
Document current symptoms, onset, duration, and progression
-
A
Allergies & Adverse Reactions
Record all allergies with specific reactions and severity
-
T
Treatments & Therapies
Note previous treatments and their effectiveness
-
I
Illnesses & Injuries
Document past medical conditions and their outcomes
-
E
Environmental Factors
Include social determinants, occupational exposures, and living conditions
-
N
Nutrition & Habits
Record dietary patterns, substance use, and lifestyle factors
-
T
Treatments That Failed
Specifically note unsuccessful treatments to avoid repetition
Common EHR Navigation Tips
Keyboard Shortcuts
- Tab: Move to the next field
- Shift + Tab: Move to the previous field
- Ctrl + S: Save in many systems
- Ctrl + Z: Undo last action
- Ctrl + F: Find/search within page
- Alt + N: Often creates a new note
- F2: Often activates editing
Documentation Efficiency
- Learn to use templates and smart phrases
- Build personal favorites lists
- Use order sets for common scenarios
- Organize notes with clear headings
- Utilize flowsheets when available
- Document progressively throughout care
- Verify auto-populated data
Finding Information
- Use patient summary screens
- Learn to filter information by date
- Use search functions effectively
- Customize views for your role
- Use graphs and trends for labs
- Access recent results quickly
- Create shortcuts to frequently used screens
Documentation Framework: SOAPIE
When documenting patient encounters in EHRs, the SOAPIE format provides a comprehensive structure:
- S: Subjective – Information reported by the patient
- O: Objective – Observable and measurable data
- A: Assessment – Analysis and interpretation of findings
- P: Plan – Proposed interventions and treatments
- I: Implementation – Specific actions taken
- E: Evaluation – Assessment of the effectiveness of interventions
This structured format ensures comprehensive documentation and supports interoperability by organizing information in a standardized way that other healthcare providers can easily navigate and understand.
8. Case Studies & Real-world Applications
Examining real-world implementations of shared care records and electronic health record systems provides valuable insights into both successful strategies and common pitfalls. These case studies illustrate how theoretical concepts translate into practical applications across different healthcare contexts.
Case Study 1: National EHR Implementation in Estonia
Background
Estonia implemented a nationwide electronic health record system in 2008, connecting all healthcare providers through a secure data exchange platform called X-Road. The system uses blockchain technology to ensure data integrity and security.
Key Features
- Patient-controlled access with digital identity cards
- Complete audit trails of all data access
- Comprehensive interoperability between all healthcare providers
- Integration with e-prescription system and health insurance
- 99% of prescriptions and 99% of medical billing handled electronically
Outcomes
- Estimated 2% of GDP saved through digitalization
- Reduced administrative burden for healthcare providers
- Improved coordination of care across providers
- Enhanced patient engagement and transparency
- Valuable population health data for research and planning
Key Success Factors
- Strong government leadership and coordination
- Established digital infrastructure and identity system
- Focus on security and patient control from the outset
- Standardized data formats and exchange protocols
- Phased implementation approach
Case Study 2: Kaiser Permanente’s Integrated EHR Implementation
Background
Kaiser Permanente, one of the largest integrated healthcare delivery systems in the United States, implemented a comprehensive EHR system (Epic) across its entire organization, connecting 39 hospitals and 700+ medical offices.
Implementation Approach
- $4 billion investment over 10 years
- Phased regional implementation with standardized core components
- Extensive clinician involvement in design and customization
- Comprehensive training program with role-specific education
- Robust technical and operational support during go-live periods
Challenges Encountered
- Initial productivity decreases during implementation phases
- Resistance from some physician groups
- Need to maintain operations during extended transition periods
- Complexity of integrating with numerous legacy systems
- Balancing standardization with local workflow needs
Outcomes
- Improved care coordination across the integrated system
- Enhanced medication safety (reduced medication errors by 50%)
- Increased preventive care delivery through systematic reminders
- Expanded telehealth and digital patient engagement capabilities
- Robust analytics supporting population health management
Case Study 3: Regional Health Information Exchange in Indiana
Background
The Indiana Health Information Exchange (IHIE) is one of the most successful regional health information exchanges in the U.S., connecting over 100 hospitals and thousands of physician practices across the state, regardless of their EHR vendor.
Key Components
- Clinical data repository aggregating information from diverse EHR systems
- Secure messaging capabilities for provider-to-provider communication
- Results delivery system for labs, imaging, and reports
- Public health reporting integration
- Population health management tools
Implementation Strategies
- Non-profit governance model with stakeholder representation
- Value-based participation incentives (not just regulatory compliance)
- Technical assistance for smaller organizations
- Standardized data agreements and consent management
- Phased service implementation starting with high-value use cases
Impact
- Estimated $26 million annual savings from reduced duplicate testing
- 90% reduction in time to obtain outside records
- Improved emergency department care through access to patient histories
- Enhanced public health surveillance capabilities
- Reduced hospital readmissions through better care coordination
Lessons Learned from Case Studies
- Leadership and Governance Matter: Clear leadership, inclusive governance structures, and stakeholder engagement are crucial for successful implementation.
- Focus on Value Creation: Implementations succeed when they deliver clear clinical and operational value, not just regulatory compliance.
- Phased Approaches Work Best: Starting with high-value, lower-complexity use cases builds momentum and confidence.
- Invest in Change Management: Technology implementation is only part of the challenge; organizational and cultural change requires significant attention.
- Standards Are Essential: Adoption of recognized standards facilitates interoperability and reduces long-term integration costs.
- User-Centered Design Improves Adoption: Systems designed with substantial clinician input achieve higher satisfaction and utilization.
9. Summary & Key Takeaways
Electronic Health Records and Shared Care Records represent a transformative approach to healthcare information management, with significant implications for nursing practice, patient care, and healthcare systems. This educational resource has explored the multifaceted aspects of these technologies, emphasizing their potential benefits, implementation challenges, and future directions.
Key Concepts Recap
Electronic Health Records
EHRs provide comprehensive digital repositories of patient health information, supporting clinical decision-making, care coordination, and administrative processes. They represent a fundamental shift from paper-based documentation to integrated digital systems that can enhance healthcare quality and efficiency.
Shared Care Records
Shared Care Records extend EHR capabilities across organizational boundaries, enabling multiple providers to access and contribute to a patient’s health information. This collaborative approach supports continuity of care and reduces information fragmentation.
Challenges in Patient History Digitization
Converting rich patient histories into computable form presents technical, semantic, and organizational challenges. Balancing structured data requirements with the need to capture nuanced clinical narratives remains a significant challenge in modern EHR design.
Interoperability Standards
Standards like HL7 FHIR are enabling unprecedented levels of interoperability between healthcare systems. These technologies support more seamless data exchange while maintaining semantic consistency and security.
Global Developments
Different countries have adopted varied approaches to EHR implementation, reflecting their healthcare system structures, cultural contexts, and policy priorities. Despite these differences, there is a global trend toward greater standardization and interoperability.
Nursing Role
Nurses play a critical role in EHR implementation and use, both as primary documenters of patient care and as stakeholders in system design. Nursing informatics continues to emerge as an important specialty at the intersection of clinical care and information technology.
Essential Considerations for Nursing Students
Educational Preparation
- Develop both technical and critical thinking skills
- Seek simulation experiences with different EHR systems
- Learn standardized terminologies (e.g., NANDA, NIC, NOC)
- Understand documentation requirements and legal implications
- Develop skills in data interpretation and visualization
Documentation Best Practices
- Document objectively and factually
- Use standardized terminology consistently
- Verify information before recording
- Balance efficiency with thoroughness
- Understand how your documentation affects interoperability
Ethical Considerations
- Maintain patient privacy and confidentiality
- Recognize biases in digital systems
- Consider equity and access issues
- Balance technology use with patient-centered care
- Advocate for systems that support nursing practice
Future Directions
The field of electronic health records continues to evolve rapidly. Emerging technologies such as artificial intelligence, natural language processing, FHIR-based APIs, and patient-generated health data will further transform healthcare documentation and information exchange. Nursing students entering the profession should prepare for a career of continuous learning and adaptation as these technologies mature and new ones emerge.
Conclusion
Electronic Health Records and Shared Care Records represent both significant opportunities and challenges for modern healthcare. By understanding the technical, organizational, and human factors involved in their implementation and use, nursing students can contribute to more effective, patient-centered care delivery. As healthcare continues its digital transformation, nurses with both clinical expertise and informatics knowledge will be increasingly valuable in shaping systems that truly support high-quality patient care.
10. References & Additional Resources
-
Argwal, R., & Craven, C. K. (2022). Electronic health records-driven phenotyping: challenges, recent advances, and perspectives. Journal of the American Medical Informatics Association, 20(e2), e206-e211. https://academic.oup.com/jamia/article-abstract/20/e2/e206/709268
-
HL7 International. (2024). FHIR Overview: Fast Healthcare Interoperability Resources. https://www.hl7.org/fhir/overview.html
-
Organisation for Economic Co-operation and Development. (2023). Progress on implementing and using electronic health record systems. https://www.oecd.org/en/publications/progress-on-implementing-and-using-electronic-health-record-systems_4f4ce846-en.html
-
HIPAA Journal. (2023). EHR Interoperability. https://www.hipaajournal.com/ehr-interoperability/
-
Fernando, B., Kalra, D., Morrison, Z., Byrne, E., & Sheikh, A. (2012). Benefits and risks of structuring and/or coding the presenting patient history in the electronic health record: systematic review. BMJ Quality & Safety, 21(4), 337-346. https://qualitysafety.bmj.com/content/21/4/337.short
-
Holmes, J. H., Beinlich, J., & Boland, M. R. (2021). Why is the electronic health record so challenging for research and clinical care? Methods of Information in Medicine. https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0041-1731784
-
Pedersen, C., & Chomutare, T. (2021). Challenges and opportunities beyond structured data in analysis of electronic health records. Wiley Interdisciplinary Reviews: Computational Statistics, 13(4), e1549. https://wires.onlinelibrary.wiley.com/doi/abs/10.1002/wics.1549
-
Orion Health. (2024). Are shared care records the key to fully integrated healthcare? https://orionhealth.com/global/blog/are-shared-care-records-the-key-to-fully-integrated-healthcare/
-
Office of the National Coordinator for Health Information Technology. (2022). What are the advantages of electronic health records? https://www.healthit.gov/faq/what-are-advantages-electronic-health-records
-
HIMSS. (2024). Interoperability in Healthcare. https://legacy.himss.org/resources/interoperability-healthcare
-
Liu, H., et al. (2022). The Impact of Electronic Health Record Interoperability on Safety and Quality of Care in High-Income Countries: Systematic Review. Journal of Medical Internet Research, 24(9), e38144. https://www.jmir.org/2022/9/e38144/
-
Galen Data. (2024). How AI Will Transform Electronic Health Records in 2025. https://galendata.com/how-will-ai-affect-electronic-health-record-systems-in-2025/
Additional Learning Resources
Online Courses and Tutorials
- Health IT Fundamentals (HealthIT.gov) – Free introductory courses on EHR concepts
- AMIA 10×10 Virtual Courses – In-depth informatics education for healthcare professionals
- Healthcare Information and Management Systems Society (HIMSS) – Certification programs and educational resources
- HL7 FHIR Foundation Tutorials – Free resources for learning FHIR standards
- OpenEHR Learning Resources – Open-source educational materials on EHR concepts
Professional Organizations
- American Nursing Informatics Association (ANIA) – Resources specific to nursing informatics
- Alliance for Nursing Informatics (ANI) – Collaborative focused on nursing’s role in healthcare informatics
- American Medical Informatics Association (AMIA) – Interdisciplinary resources on health informatics
- International Medical Informatics Association – Nursing Informatics Special Interest Group (IMIA-NI)
- Healthcare Information and Management Systems Society (HIMSS)
Simulation Resources
- EHR Go – Educational EHR platform designed for nursing and health professions education
- SimChart – Clinical simulation tool for nursing students
- DocuCare – Simulated EHR system for educational purposes
- TIGER Virtual Learning Environment – Technology Informatics Guiding Education Reform resources
- Open-source EHR sandboxes for practice with various systems
Books and Journals
- Journal of the American Medical Informatics Association (JAMIA)
- CIN: Computers, Informatics, Nursing journal
- Health Informatics: An Interprofessional Approach (Nelson & Staggers)
- Nursing Informatics: Where Technology and Caring Meet (Ball et al.)
- Electronic Health Records: Challenges in Design and Implementation (Sittig)
Accessing EHR Vendor Resources
Many major EHR vendors offer free educational resources, webinars, and documentation that can help nursing students understand specific systems:
- Epic – UserWeb (requires institutional access) or public YouTube training videos
- Cerner – Cerner Learning resources and documentation
- Meditech – Customer briefings and educational materials
- Allscripts – Client Connect portal resources
- NextGen – NextGen Healthcare University
Consider reaching out to your clinical placement sites to inquire about access to training materials for the systems you’ll be using in practice.