Care of Eyes in Nursing
Essential Practices for Patient Comfort, Hygiene & Vision Health
Introduction to Eye Care in Nursing
Eye care represents one of the most crucial aspects of comprehensive nursing practice, directly impacting patient comfort, preventing complications, and maintaining optimal vision health. As healthcare professionals, nurses play an essential role in delivering specialized eye care that encompasses assessment, hygiene maintenance, medication administration, and patient education. This comprehensive guide explores evidence-based practices for effective eye care in nursing, providing you with the knowledge and skills necessary to deliver exceptional patient outcomes.
The significance of proper eye care extends beyond basic hygiene – it encompasses infection prevention, comfort enhancement, and vision preservation. Through systematic assessment and appropriate interventions, nurses can identify potential complications early and implement preventive measures that significantly improve patient experiences and clinical outcomes.
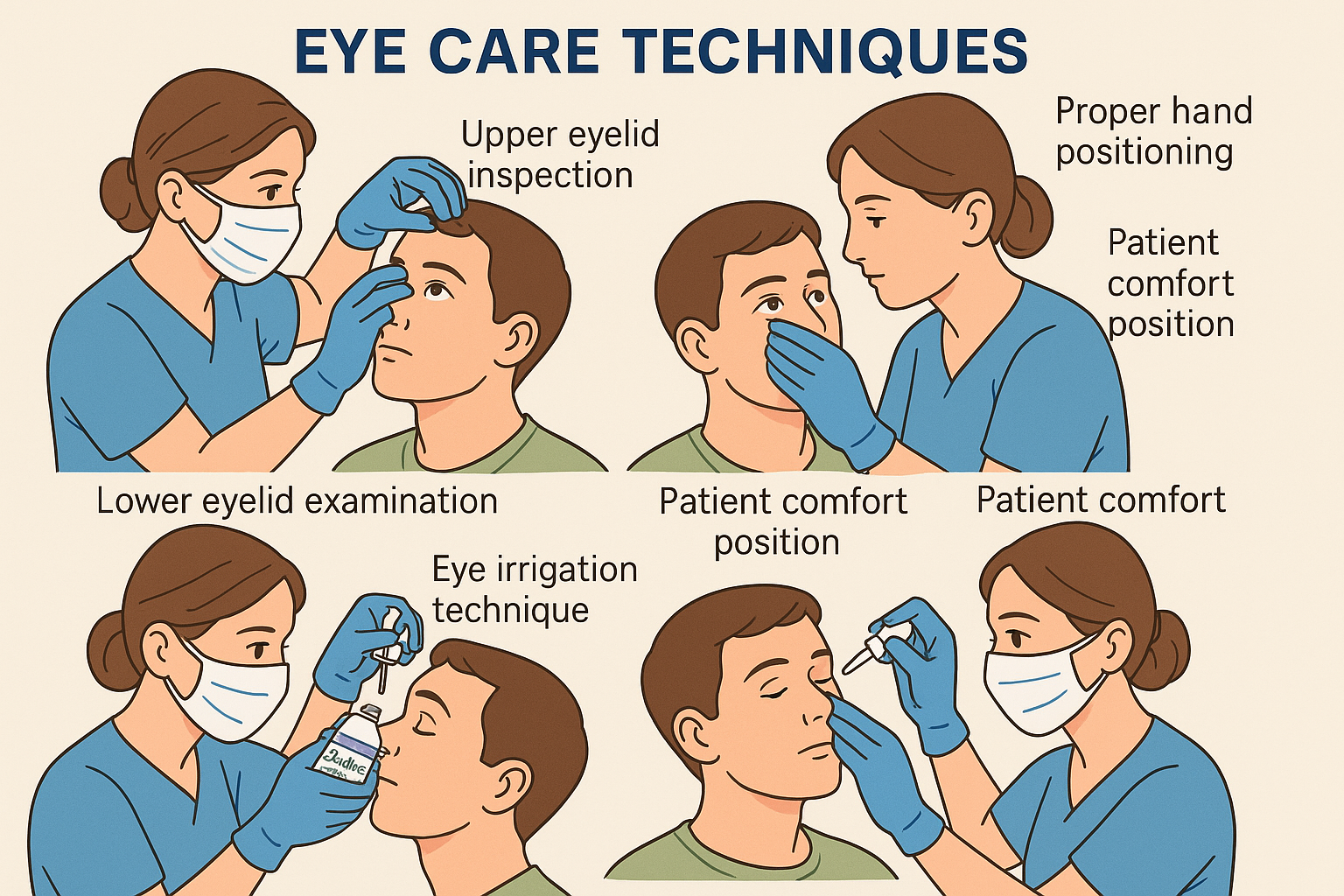
Professional eye care techniques for nursing practice
1. Anatomy and Physiology Overview
Understanding ocular anatomy forms the foundation of effective eye care nursing practice. The eye is a complex organ system requiring specialized knowledge for proper assessment and intervention. Each anatomical structure plays a crucial role in vision and eye health maintenance.
| Structure | Function | Nursing Considerations |
|---|---|---|
| Cornea | Light refraction and protection | Monitor for clarity, abrasions, and infections |
| Conjunctiva | Lubrication and protection | Assess for inflammation, discharge, and irritation |
| Sclera | Structural support and protection | Observe for discoloration and surface changes |
| Iris | Light regulation through pupil control | Evaluate pupil response and symmetry |
| Lens | Focus adjustment for vision | Monitor for cloudiness and accommodation |
| Eyelids | Protection and tear distribution | Assess for swelling, lesions, and proper closure |
Memory Aid: CASTLE
Cornea – Clear window for light
Anterior chamber – Aqueous humor space
Sclera – Strong outer layer
Tear film – Protective moisture
Lens – Light focusing structure
Eyelids – External protection barriers
2. Comprehensive Eye Assessment
Systematic eye assessment is fundamental to effective eye care nursing practice. A thorough evaluation encompasses visual inspection, functional testing, and documentation of findings. This comprehensive approach enables early detection of problems and appropriate intervention planning.
Assessment Components
- Visual acuity testing
- External eye examination
- Pupil response evaluation
- Extraocular movement assessment
- Intraocular pressure considerations
- Symptom documentation
Step-by-Step Assessment Protocol
Visual Inspection
- • Assess eyelid position and symmetry
- • Examine conjunctiva for redness or discharge
- • Evaluate sclera coloration
- • Check for foreign bodies or lesions
- • Observe tear production and distribution
Functional Testing
- • Test pupil response to light
- • Assess accommodation reflexes
- • Evaluate extraocular movements
- • Check visual field responses
- • Document any pain or discomfort
Critical Assessment Findings
Immediate attention required for: sudden vision changes, severe pain, light sensitivity, halos around lights, flashing lights, curtain-like vision loss, or significant eye trauma. These findings may indicate serious conditions requiring urgent medical intervention.
Memory Aid: VISION
Visual acuity – Test clarity
Inspection – External examination
Symmetry – Compare both eyes
Intraocular – Consider pressure
Ocular movements – Test function
Neurological – Pupil responses
3. Eye Hygiene and Cleansing
Proper eye hygiene forms the cornerstone of effective eye care nursing practice. Maintaining ocular cleanliness prevents infections, reduces discomfort, and promotes healing. This section covers essential techniques for safe and effective eye cleansing procedures.
| Cleansing Solution | Indications | Precautions |
|---|---|---|
| Sterile Normal Saline | General cleansing, irrigation, routine care | Use sterile technique, room temperature |
| Sterile Water | Emergency irrigation, basic cleansing | Not for prolonged use, isotonic preferred |
| Prescribed Eye Wash | Specific conditions, medication orders | Follow exact instructions, monitor reactions |
| Balanced Salt Solution | Surgical procedures, specialized care | Maintain sterility, proper storage |
Essential Cleansing Procedure
Step-by-Step Protocol
- 1. Perform hand hygiene and don appropriate PPE
- 2. Explain procedure to patient and ensure comfort
- 3. Position patient appropriately (sitting or supine)
- 4. Prepare sterile cleansing solution at room temperature
- 5. Use sterile cotton balls or gauze pads
- 6. Cleanse from inner to outer canthus
- 7. Use each cotton ball only once
- 8. Gently dry with clean, dry gauze
- 9. Document procedure and patient response
- 10. Dispose of materials appropriately
Best Practices
- • Always use sterile technique
- • Maintain gentle pressure
- • Work from clean to dirty areas
- • Never reuse cleansing materials
- • Monitor for patient discomfort
- • Document all findings
Critical Precautions
- • Avoid excessive pressure
- • Never use soap or detergents
- • Avoid cotton swabs on cornea
- • Stop if patient reports pain
- • Watch for allergic reactions
- • Maintain sterile field integrity
4. Medication Administration
Ophthalmic medication administration requires specialized knowledge and precise technique to ensure therapeutic effectiveness and patient safety. Eye care nursing involves understanding various medication forms, proper administration methods, and monitoring for therapeutic responses and adverse effects.
| Medication Type | Administration Method | Key Considerations |
|---|---|---|
| Eye Drops | Instillation into lower conjunctival sac | Avoid touching dropper to eye, one drop at a time |
| Eye Ointments | Ribbon application to lower lid | May cause temporary vision blurring |
| Gel Formulations | Similar to drops but slower release | Longer contact time, less frequent dosing |
| Inserts | Placement in conjunctival sac | Specialized placement technique required |
Eye Drop Administration Technique
Proper Instillation Method
- 1. Verify patient identity and medication order
- 2. Perform hand hygiene and check medication expiration
- 3. Position patient comfortably with head tilted back
- 4. Gently pull down lower eyelid to create pocket
- 5. Hold dropper 1-2 cm above conjunctival sac
- 6. Instill prescribed number of drops
- 7. Ask patient to close eyes gently
- 8. Apply gentle pressure to nasolacrimal duct
- 9. Wait 5 minutes between different medications
- 10. Document administration and patient response
Safety Measures
- • Always use sterile technique
- • Check for allergies before administration
- • Monitor for immediate reactions
- • Never share eye medications
- • Store medications properly
- • Replace medications after eye infections
Common Errors to Avoid
- • Touching dropper to eye surface
- • Administering too many drops
- • Skipping nasolacrimal pressure
- • Inadequate spacing between medications
- • Using expired medications
- • Contaminating medication containers
Memory Aid: DROPS
Direction – Lower conjunctival sac
Room temperature – Warm medications
One drop – Single drop per instillation
Pressure – Nasolacrimal duct compression
Spacing – Five minutes between medications
5. Eye Irrigation Techniques
Eye irrigation is a critical skill in eye care nursing, used for removing foreign substances, cleansing infected eyes, and providing comfort. Proper technique ensures effective treatment while preventing further injury or contamination.
Indications for Eye Irrigation
- Chemical exposure
- Foreign body removal
- Infection treatment
- Allergic reactions
- Excessive discharge
- Medication preparation
- Comfort enhancement
- Surgical preparation
Irrigation Procedure
| Step | Action | Rationale |
|---|---|---|
| 1 | Gather sterile irrigation solution and equipment | Ensures sterility and prevents contamination |
| 2 | Position patient with affected eye downward | Prevents cross-contamination to unaffected eye |
| 3 | Direct flow from inner to outer canthus | Natural drainage pattern, comfort |
| 4 | Maintain steady, gentle pressure | Effective cleansing without tissue damage |
| 5 | Continue until return is clear | Ensures complete removal of contaminants |
Essential Equipment
- • Sterile irrigation solution (saline preferred)
- • Sterile irrigation syringe or tubing
- • Sterile basin for collection
- • Sterile gauze pads
- • Protective eyewear for nurse
- • Towels for patient comfort
Emergency Considerations
- • Chemical burns require immediate irrigation
- • Continue for 15-20 minutes minimum
- • Do not delay for equipment preparation
- • Use any available clean water initially
- • Call for emergency assistance
- • Document time and duration
Memory Aid: FLUSH
Flow direction – Inner to outer canthus
Low pressure – Gentle stream
Unaffected eye – Protect from contamination
Sterile solution – Maintain asepsis
Hold eyelids – Expose conjunctival sac
6. Eye Protection and Safety
Implementing comprehensive eye protection strategies is essential for maintaining patient safety and preventing vision-threatening complications. Effective eye care nursing includes understanding various protective measures and their appropriate applications.
| Protection Method | Application | Duration |
|---|---|---|
| Eye Shields | Post-surgical protection, trauma cases | As ordered, typically 24-48 hours |
| Moisture Chambers | Dry eye conditions, corneal protection | Continuous during treatment period |
| Eye Patches | Corneal abrasions, forced rest | 12-24 hours, monitor closely |
| Protective Eyewear | Chemical exposure risk, UV protection | During exposure risk periods |
Environmental Safety Measures
Hospital Environment
- • Proper lighting levels
- • Clean air circulation
- • Humidity control
- • Reduced glare sources
- • Safe mobility pathways
- • Emergency equipment accessibility
Personal Protection
- • Hand hygiene protocols
- • Sterile technique maintenance
- • Appropriate PPE usage
- • Cross-contamination prevention
- • Equipment sterilization
- • Infection control measures
High-Risk Situations
Certain patient conditions and procedures require heightened protective measures in eye care nursing:
- • Immunocompromised patients
- • Post-operative eye surgery
- • Chemical exposure incidents
- • Infectious conjunctivitis
- • Trauma with foreign bodies
- • Radiation exposure history
Memory Aid: PROTECT
Prevention – Primary focus
Risk assessment – Identify hazards
Observation – Monitor continuously
Technology – Use appropriate devices
Education – Patient and family teaching
Cleanliness – Maintain sterile conditions
Timing – Prompt intervention
7. Common Complications and Management
Understanding potential complications in eye care nursing is crucial for early recognition and appropriate intervention. Prompt identification and management of complications can prevent serious vision-threatening outcomes and ensure optimal patient recovery.
| Complication | Signs & Symptoms | Immediate Actions |
|---|---|---|
| Infection | Redness, discharge, pain, swelling | Isolate, culture, antibiotic therapy |
| Corneal Abrasion | Severe pain, tearing, light sensitivity | Protect eye, pain management, healing promotion |
| Chemical Burn | Severe pain, vision changes, tissue damage | Immediate irrigation, emergency care |
| Allergic Reaction | Itching, swelling, rash, difficulty breathing | Discontinue agent, antihistamines, monitor |
| Increased Pressure | Eye pain, nausea, vision changes, halos | Immediate medical evaluation, pressure reduction |
Prevention Strategies
Infection Prevention
- • Strict hand hygiene
- • Sterile technique
- • Equipment sterilization
- • Proper medication storage
- • Patient isolation when needed
Injury Prevention
- • Protective eyewear
- • Safe environment
- • Proper positioning
- • Gentle techniques
- • Patient education
Allergy Prevention
- • Allergy screening
- • Medication reviews
- • Patch testing
- • Emergency preparedness
- • Documentation
Emergency Response Protocol
- 1. Assess severity and stabilize patient
- 2. Implement immediate interventions
- 3. Notify physician or emergency services
- 4. Document all findings and actions
- 5. Continue monitoring and support
- 6. Provide patient and family education
Memory Aid: RESCUE
Recognize – Early identification
Evaluate – Assess severity
Stabilize – Immediate care
Call – Get help promptly
Understand – Know protocols
Educate – Prevent recurrence
8. Best Practices Worldwide
Learning from global innovations in eye care nursing helps improve patient outcomes and advance professional practice. These international best practices demonstrate excellence in eye care delivery and can be adapted to various healthcare settings.
Scandinavian Model
Nordic countries emphasize preventive eye care nursing with comprehensive screening programs and patient education initiatives.
- • Systematic patient education protocols
- • Integrated technology for monitoring
- • Multidisciplinary team approaches
- • Evidence-based practice guidelines
- • Continuous quality improvement
Japanese Approach
Japan’s eye care nursing focuses on precision, gentleness, and respect for patient dignity with innovative techniques.
- • Meticulous attention to detail
- • Advanced sterile techniques
- • Patient comfort prioritization
- • Technology integration
- • Continuous professional development
| Country/Region | Innovation | Application |
|---|---|---|
| United Kingdom | Standardized assessment protocols | Consistent quality across healthcare systems |
| Australia | Telehealth eye care monitoring | Remote patient support and follow-up |
| Canada | Indigenous community programs | Culturally sensitive eye care delivery |
| Netherlands | Patient-centered care models | Individualized treatment approaches |
| Singapore | AI-assisted diagnostics | Enhanced accuracy and efficiency |
Implementation Considerations
When adopting international best practices in eye care nursing, consider:
- • Cultural and regulatory differences
- • Resource availability and constraints
- • Staff training and education needs
- • Technology infrastructure requirements
- • Patient population characteristics
- • Cost-effectiveness analysis
Memory Aid: GLOBAL
Guidelines – Follow evidence-based protocols
Learning – Continuous education
Optimization – Improve processes
Best practices – Adopt proven methods
Adaptation – Modify for local needs
Leadership – Champion improvements
Conclusion
Mastering eye care nursing requires dedication to excellence, continuous learning, and commitment to patient safety. The comprehensive knowledge and skills outlined in this guide provide the foundation for delivering exceptional eye care that promotes patient comfort, prevents complications, and preserves vision health.
Remember that effective eye care nursing extends beyond technical skills to encompass compassionate patient interaction, thorough assessment, and proactive prevention strategies. By implementing these evidence-based practices and maintaining high standards of care, you contribute significantly to positive patient outcomes and professional excellence in healthcare.
Key Takeaways for Excellence
- • Prioritize patient safety and comfort in all procedures
- • Maintain strict sterile technique and infection control
- • Develop systematic assessment and documentation skills
- • Stay current with evidence-based practices and innovations
- • Foster therapeutic relationships through education and support
- • Continuously improve your eye care nursing competencies
Excellence in eye care nursing transforms lives by preserving vision and enhancing quality of life for patients worldwide.
