Incidents and Adverse Events in Nursing
Complete Guide to Patient Safety Management
Table of Contents
Introduction to Patient Safety
Why This Matters
Patient safety is the cornerstone of quality healthcare delivery. Every healthcare professional, especially nurses who spend the most time with patients, must understand how to identify, manage, and prevent incidents that could compromise patient wellbeing. An incident in healthcare settings can range from medication errors to equipment failures, each requiring systematic approach for resolution and prevention.
Remember: Every incident is a learning opportunity to improve patient care and prevent future occurrences.
Learning Objectives
- Master incident identification and classification techniques
- Develop systematic approach to Root Cause Analysis
- Implement effective CAPA strategies
- Write professional incident reports
- Apply international best practices
Global Patient Safety Statistics
Understanding Incidents & Adverse Events
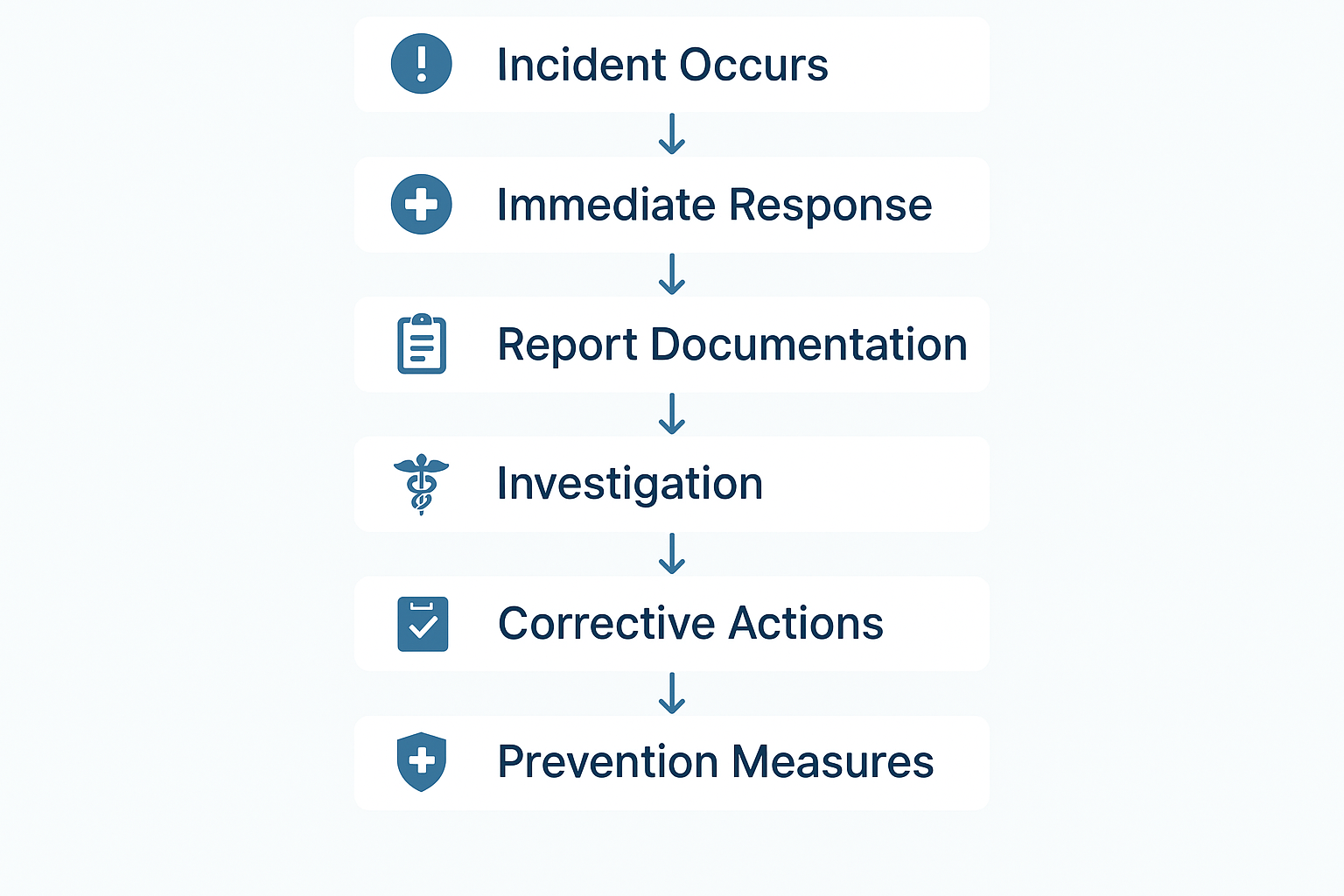
Healthcare Incident Reporting Process Flow
Adverse Events
An unintended injury resulting from medical care that causes measurable harm to the patient.
Characteristics:
- Results in patient harm
- Requires additional treatment
- May cause permanent disability
- Can lead to death
Incidents
Any deviation from normal operations or expected outcomes that has the potential to cause harm.
Types:
- Near misses (no harm occurred)
- No-harm events
- Unsafe conditions
- System failures
Incident Classification Matrix
| Severity Level | Description | Examples | Response Time |
|---|---|---|---|
| Level 1 – Critical | Death or severe permanent harm | Medication overdose causing death, surgical errors | Immediate (0-24 hours) |
| Level 2 – Major | Moderate harm requiring intervention | Patient falls resulting in fractures, wrong medication | Within 48 hours |
| Level 3 – Minor | Minimal harm or near miss | Minor skin tears, delayed medication | Within 72 hours |
| Level 4 – Near Miss | No harm occurred but potential existed | Wrong patient ID caught before procedure | Within 1 week |
Memory Aid: SAFER Incident Assessment
Capturing Incidents
Detection
- Active surveillance
- Staff reporting
- Patient complaints
- Automated alerts
Documentation
- Immediate recording
- Detailed description
- Witness statements
- Photographic evidence
Communication
- Immediate supervisor
- Risk management
- Medical team
- Family notification
Step-by-Step Incident Capture Process
Immediate Response
Ensure patient safety first. Provide immediate care and stabilize the situation.
Timeline: Within 5 minutes of incident discovery
Secure the Scene
Preserve evidence and prevent further incidents. Document environmental factors.
Key: Maintain scene integrity for investigation
Initial Documentation
Record facts objectively without assigning blame. Use the incident report form.
Remember: Facts only, no opinions or assumptions
Notification Chain
Notify appropriate personnel according to incident severity and organizational policy.
Critical: Follow notification hierarchy promptly
Overcoming Reporting Barriers
Common Barriers:
- Fear of blame or punishment
- Time constraints
- Uncertainty about what to report
- Complex reporting systems
Solutions:
- Just culture environment
- Simplified reporting tools
- Clear reporting guidelines
- Regular training and feedback
Root Cause Analysis (RCA)
What is Root Cause Analysis?
Root Cause Analysis is a systematic investigation technique used to identify the underlying causes of an incident or adverse event. Rather than focusing on immediate causes or individual blame, RCA examines system failures and organizational factors that contributed to the incident occurrence.
Key Principle
“People do not come to work to cause harm. When an incident occurs, we must look beyond individual actions to understand the system factors that influenced those actions.”
5 Whys Technique
Example: Medication Error
Why 1: Patient received wrong medication
Why 2: Nurse picked up wrong syringe
Why 3: Similar-looking medications stored together
Why 4: No color-coding system implemented
Why 5: Storage policy outdated and not reviewed
Fishbone Diagram
Six Categories:
RCA Process Framework
Team Formation
Assemble multidisciplinary team with relevant expertise
Data Collection
Gather comprehensive information about the incident
Analysis
Apply systematic analysis techniques to identify causes
Recommendations
Develop actionable recommendations for improvement
RCA Timeline
RCA Team Composition
Memory Aid: REACT Framework for RCA
Corrective and Preventive Actions (CAPA)
Understanding CAPA
CAPA is a systematic approach to address root causes identified through incident analysis. It involves implementing corrective actions to fix immediate problems and preventive actions to stop similar incidents from occurring in the future.
Corrective Actions
Address immediate causes and fix current problems
- Repair faulty equipment
- Retrain involved staff
- Update procedures
Preventive Actions
Prevent similar incidents from occurring
- System-wide policy changes
- Enhanced monitoring systems
- Proactive risk assessments
CAPA Implementation Process
1. Action Planning
Develop specific, measurable, achievable, relevant, and time-bound (SMART) actions.
SMART Criteria:
2. Resource Allocation
Ensure adequate resources (human, financial, technological) are available.
Human Resources
Financial Resources
Technology Resources
3. Implementation
Execute actions according to the established timeline and monitor progress.
4. Effectiveness Evaluation
Measure the impact of implemented actions on reducing incident recurrence.
Key Metrics:
- • Incident recurrence rate
- • Time to resolution
- • Staff compliance rates
- • Patient satisfaction scores
CAPA Action Categories
| Category | Description | Examples | Timeline |
|---|---|---|---|
| Immediate | Actions to address immediate safety concerns | Equipment isolation, staff redeployment | 0-24 hours |
| Short-term | Quick fixes and temporary solutions | Procedure updates, additional supervision | 1-30 days |
| Long-term | Systematic improvements and redesign | System upgrades, culture change initiatives | 1-12 months |
| Strategic | Organizational and policy-level changes | New technology implementation, structural changes | 6 months – 2 years |
Success Factors
- Leadership Support: Visible commitment from management
- Clear Accountability: Defined roles and responsibilities
- Regular Monitoring: Ongoing tracking of progress
- Staff Engagement: Involving frontline staff in solutions
Common Pitfalls
- Quick Fixes: Addressing symptoms rather than root causes
- Lack of Follow-up: Not monitoring effectiveness
- Resource Constraints: Inadequate support for implementation
- Resistance to Change: Poor change management
Professional Report Writing
The Art of Incident Reporting
Effective incident reporting is crucial for patient safety improvement. A well-written report provides clear, objective information that enables proper analysis and prevents similar incidents. Every incident report should tell a complete story while maintaining professional standards and legal compliance.
Golden Rule of Incident Reporting
“Write as if the report will be read by the patient, their family, a lawyer, and a quality improvement team – because it might be.”
Report Structure Framework
1. Header Information
- • Report ID number
- • Date and time of incident
- • Location details
- • Reporter information
- • Patient identifiers
- • Incident category
2. Incident Description
Objective, chronological account of events
Template Structure:
What: Description of the incident
When: Specific timing
Where: Exact location
Who: People involved
How: Sequence of events
3. Contributing Factors
Environmental and system factors that may have contributed
4. Immediate Actions
Steps taken immediately following the incident
- • Patient care provided
- • Notifications made
- • Scene preservation
5. Outcome and Follow-up
Patient condition and planned actions
Next Steps: Planned interventions and monitoring
Do’s
- Use objective language: Stick to observable facts
- Be specific: Include exact times, measurements, locations
- Use direct quotes: When documenting patient/witness statements
- Write legibly: Use clear, professional language
- Document promptly: Write while memory is fresh
Don’ts
- Avoid blame: Don’t assign fault or responsibility
- No speculation: Don’t guess or assume causes
- Avoid opinions: Don’t include personal judgments
- Don’t use abbreviations: Write out terms completely
- Never alter records: Don’t change or white-out entries
Sample Incident Report
Incident Description:
At approximately 14:30 on 03/15/2024, patient Mrs. Johnson (Room 302A) was found on the floor beside her bed by this writer. Patient was conscious and oriented, stating “I was trying to get to the bathroom and my legs gave out.” Patient was assisted to a sitting position on the floor. No visible injuries noted initially. Bed rails were in the down position. Call light was within reach but not activated.
Contributing Factors:
Patient had received pain medication (morphine 2mg IV) at 13:45. Room lighting was adequate. Floor was dry. Patient wearing non-slip socks. Previous fall risk assessment score: 8/10 (high risk).
Immediate Actions:
Dr. Williams notified at 14:35. Full body assessment completed – no injuries found. Vital signs stable. Bed alarm activated. Fall risk interventions reinforced with patient and family.
Legal and Ethical Considerations
Legal Protection:
- Quality assurance privilege
- Peer review protection
- Root cause analysis privilege
Ethical Obligations:
- Patient safety first
- Transparency and honesty
- Continuous improvement
Global Best Practices
Learning from International Leaders
Healthcare organizations worldwide have developed innovative approaches to incident management and patient safety. These best practices demonstrate how systematic approaches to incident reporting and analysis can significantly improve patient outcomes and organizational learning.
United States – AHRQ PSNET
The Agency for Healthcare Research and Quality (AHRQ) Patient Safety Network represents a comprehensive approach to patient safety education and incident prevention.
National web-based resource providing evidence-based patient safety information and tools.
Standardized incident reporting across 4,000+ healthcare facilities nationwide.
Australia – AIMS Program
The Australian Incident Monitoring System (AIMS) pioneered anonymous incident reporting with a focus on system improvement rather than individual blame.
Anonymous reporting system with rapid feedback to reporting institutions.
40% reduction in preventable adverse events over 10 years.
United Kingdom – NRLS
The National Reporting and Learning System (NRLS) established a centralized approach to incident reporting across the National Health Service.
Centralized database with advanced analytics for pattern recognition.
Over 2 million incident reports annually, driving systematic improvements.
Switzerland – Critical Incident Reporting
Swiss hospitals developed a unique approach combining mandatory reporting with voluntary peer review networks.
Hybrid system combining mandatory and voluntary reporting with peer networks.
Enhanced interprofessional collaboration and shared learning culture.
Common Success Factors Across Countries
| Success Factor | USA | Australia | UK | Switzerland |
|---|---|---|---|---|
| Leadership Support | ||||
| Just Culture | ||||
| Technology Integration | ||||
| Feedback Mechanisms |
Emerging Innovations in Incident Management
Artificial Intelligence
- • Predictive analytics for incident prevention
- • Natural language processing for report analysis
- • Pattern recognition in large datasets
- • Automated risk scoring systems
Mobile Technology
- • Real-time incident reporting apps
- • Photo and video documentation
- • Voice-to-text reporting capabilities
- • Immediate notification systems
Implementation Roadmap for Your Organization
Assessment Phase (Months 1-2)
- • Evaluate current incident reporting processes
- • Identify gaps and improvement opportunities
- • Benchmark against international standards
Planning Phase (Months 3-4)
- • Develop implementation strategy
- • Secure leadership support and resources
- • Design training programs
Implementation Phase (Months 5-12)
- • Roll out new systems and processes
- • Provide comprehensive staff training
- • Monitor adoption and effectiveness
Evaluation Phase (Ongoing)
- • Measure outcomes and impact
- • Continuous improvement initiatives
- • Share learnings with broader community
Conclusion & Key Takeaways
Mastering Incident Management
Effective incident management is not just about reporting events—it’s about creating a culture of safety, learning, and continuous improvement. As future nurses, your role in this system is crucial for protecting patients and advancing healthcare quality. Every incident you properly identify, report, and analyze contributes to a safer healthcare environment for all.
Essential Principles
- Patient safety first: Always prioritize immediate patient care before documentation
- Just culture mindset: Focus on system improvement, not individual blame
- Objective reporting: Document facts without assumptions or opinions
- Systematic analysis: Use structured approaches like RCA for investigation
Action Steps
- Practice reporting: Use simulation scenarios to build confidence
- Learn your system: Understand your organization’s specific processes
- Stay updated: Keep current with best practices and regulations
- Advocate for safety: Speak up when you see potential risks
Final Memory Aid: SAFETY Framework
The Future of Patient Safety
As healthcare continues to evolve with new technologies, treatments, and challenges, the principles of incident management remain constant. Your generation of nurses will lead the next wave of patient safety innovations, building on the foundation of systematic incident reporting, thorough analysis, and effective corrective actions.
“The goal is not to prevent all adverse events—that’s impossible. The goal is to learn from every incident to make healthcare safer for everyone.”
– Institute for Healthcare Improvement