Nursing Care for Pressure Points: Assessment & Management
Using Braden and Norton Scales for Comprehensive Patient Care
Table of Contents
Introduction to Pressure Point Care
Pressure point care represents one of the most critical aspects of modern nursing practice, directly impacting patient outcomes and quality of life. As healthcare professionals, understanding the complexities of pressure injury assessment and management is essential for providing comprehensive patient care. This comprehensive guide explores evidence-based approaches to pressure point care using standardized assessment tools that have revolutionized patient safety protocols worldwide.
Critical Statistics
- 2.5 million pressure injuries occur annually in US acute care facilities
- 60,000 deaths are attributed to pressure injury complications yearly
- $9.1-11.6 billion annual healthcare costs related to pressure injuries
- 95% of pressure injuries are preventable with proper care
Learning Objectives
- Master pressure point assessment techniques
- Utilize Braden and Norton scales effectively
- Implement evidence-based prevention strategies
- Develop comprehensive care plans for at-risk patients
Why Pressure Point Care Matters
Effective pressure point care goes beyond preventing wounds—it preserves patient dignity, reduces healthcare costs, prevents complications, and demonstrates the highest standard of professional nursing practice. Every assessment and intervention contributes to improved patient outcomes and quality of life.
Anatomy and Physiology of Pressure Points
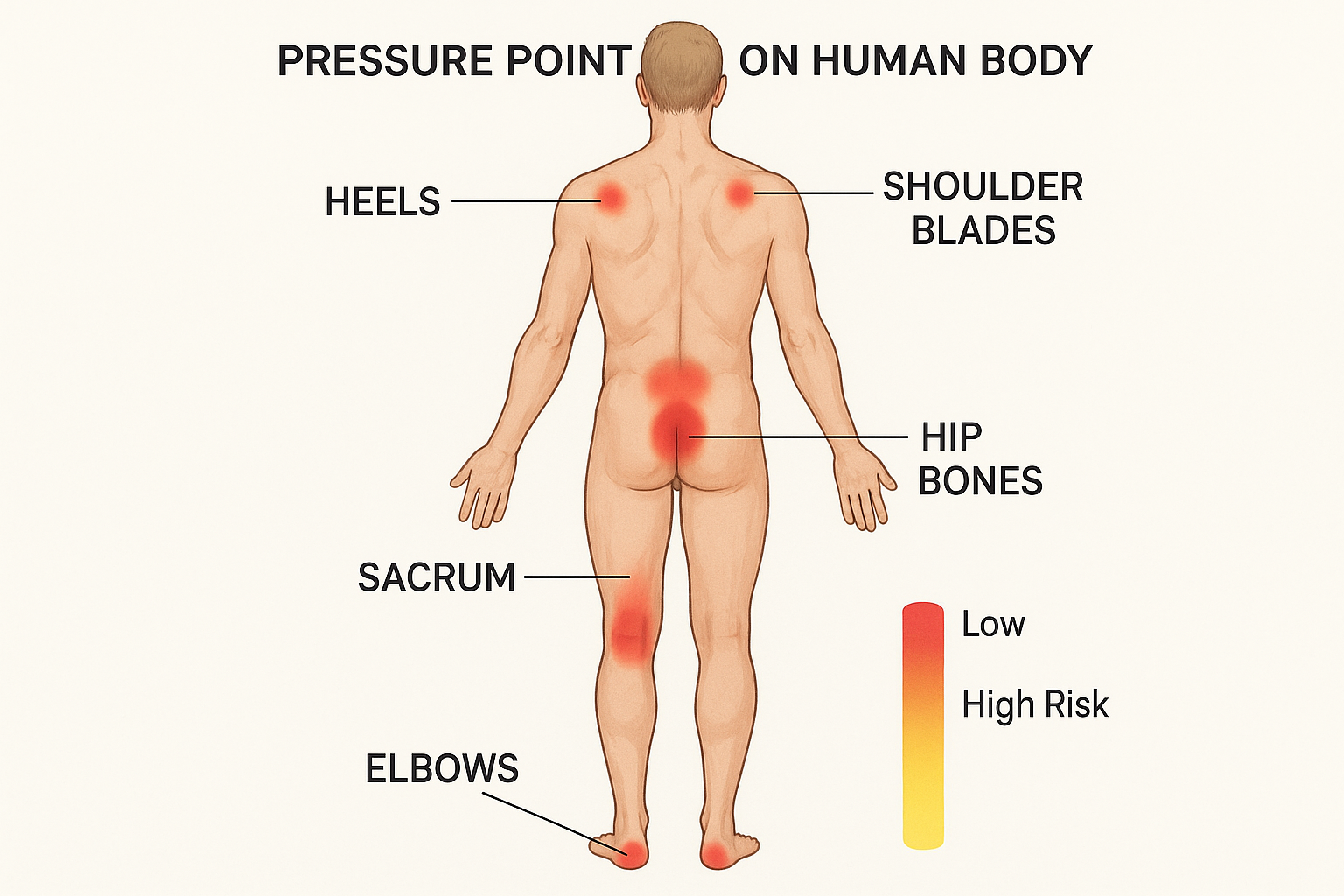
Anatomical diagram showing common pressure points and risk areas for pressure injury development
Skin Structure and Vulnerability
The skin consists of multiple layers that work together to protect underlying structures. Understanding these layers is crucial for effective pressure point care:
- Epidermis: Outer protective layer, most susceptible to friction and shear forces
- Dermis: Contains blood vessels, nerves, and structural proteins
- Subcutaneous tissue: Provides cushioning and insulation
- Deep fascia and muscle: Underlying structures affected by prolonged pressure
Pressure and Circulation
Normal capillary pressure ranges from 12-32 mmHg. When external pressure exceeds this threshold, blood flow becomes compromised, leading to tissue hypoxia and potential cell death.
Critical Pressure Thresholds:
- • 32 mmHg: Capillary occlusion begins
- • 70 mmHg: Complete blood flow cessation
- • 2 hours: Irreversible tissue damage timeline
- • 6 hours: Deep tissue injury development
Memory Aid: “PRESSURE” Mnemonic
P – Positioning every 2 hours
R – Risk assessment using scales
E – Examine skin integrity daily
S – Support surfaces and cushioning
S – Skin care and hygiene
U – Understand patient limitations
R – Record all findings accurately
E – Educate patient and family
Risk Factors and Pathophysiology
Understanding risk factors is fundamental to effective pressure point care. Multiple factors contribute to pressure injury development, and recognizing these elements enables proactive intervention and prevention strategies.
Intrinsic Factors
- • Advanced age (>65 years)
- • Immobility or limited mobility
- • Decreased sensation
- • Poor nutrition and hydration
- • Chronic medical conditions
- • Decreased perfusion
- • Cognitive impairment
- • Incontinence
Extrinsic Factors
- • Prolonged pressure
- • Friction and shear forces
- • Moisture exposure
- • Hard surfaces
- • Medical devices
- • Inadequate positioning
- • Poor skin care
- • Environmental factors
Healthcare-Related
- • Surgical procedures
- • ICU stays
- • Sedation and anesthesia
- • Mechanical ventilation
- • Vasopressor medications
- • Steroid therapy
- • Inadequate staffing
- • Equipment-related pressure
Clinical Insight: The Pressure Injury Cascade
Pressure injuries develop through a predictable cascade: Pressure → Ischemia → Inflammation → Tissue Breakdown → Wound Formation. Understanding this progression allows nurses to intervene at any stage to prevent advancement.
Key Timing Factors:
- • 30 minutes: Initial tissue response to pressure
- • 2 hours: Maximum safe pressure duration
- • 6 hours: Deep tissue injury threshold
- • 24-48 hours: Visible skin changes appear
Comprehensive Assessment Techniques
Systematic assessment forms the foundation of effective pressure point care. A thorough evaluation encompasses multiple domains including physical examination, risk assessment, and ongoing monitoring protocols that ensure comprehensive patient safety.
Visual Inspection Protocol
Step-by-Step Assessment:
- Inspect skin during routine care activities
- Use adequate lighting for thorough examination
- Examine all bony prominences systematically
- Look for changes in skin color, temperature, texture
- Document all findings with precise descriptions
- Compare to previous assessments for changes
Warning Signs to Assess:
- • Non-blanchable erythema
- • Skin discoloration
- • Warmth or coolness
- • Edema or induration
- • Pain or tenderness
- • Skin breakdown or blistering
Palpation Techniques
Palpation Assessment:
- Temperature: Compare bilateral symmetry
- Turgor: Assess skin elasticity and hydration
- Texture: Feel for roughness or smoothness
- Moisture: Evaluate for dryness or excessive moisture
- Blanching: Test capillary refill response
- Edema: Check for fluid accumulation
Blanching Test Procedure:
- Apply firm finger pressure for 3 seconds
- Release pressure and observe skin response
- Normal: Immediate return to baseline color
- Abnormal: Delayed or absent blanching response
- Document findings and compare to baseline
Best Practice: Structured Assessment Framework
Implement a systematic approach using the “SAFER-R” assessment framework for consistent pressure point care evaluation:
S – Skin assessment and integrity
A – Activity and mobility evaluation
F – Friction and shear risk factors
E – Exposure to moisture assessment
R – Risk factor identification
– (hyphen) Reassessment intervals
R – Recording and documentation
Braden Scale Assessment
The Braden Scale, developed by Barbara Braden and Nancy Bergstrom in 1987, represents the most widely used pressure injury risk assessment tool globally. This evidence-based instrument evaluates six critical domains that influence pressure point care outcomes and provides a standardized approach to risk stratification.
Scale Overview
- Score Range: 6-23 points
- Assessment Frequency: Every 24-48 hours
- Validity: 83-100% predictive accuracy
- Reliability: Inter-rater reliability >0.90
- Risk Categories: 4 distinct levels
- Implementation: Widely adopted globally
Risk Stratification
High Risk: ≤12 points
Requires intensive interventions
Moderate Risk: 13-14 points
Implement prevention protocols
Mild Risk: 15-18 points
Monitor and maintain precautions
Low Risk: 19-23 points
Routine care with monitoring
Complete Braden Scale Assessment Matrix
| Domain | 1 Point | 2 Points | 3 Points | 4 Points | Clinical Significance |
|---|---|---|---|---|---|
| Sensory Perception | Completely Limited | Very Limited | Slightly Limited | No Impairment | Ability to respond meaningfully to pressure-related discomfort |
| Moisture | Constantly Moist | Very Moist | Occasionally Moist | Rarely Moist | Degree to which skin is exposed to moisture |
| Activity | Bedfast | Chairfast | Walks Occasionally | Walks Frequently | Degree of physical activity |
| Mobility | Completely Immobile | Very Limited | Slightly Limited | No Limitation | Ability to change and control body position |
| Nutrition | Very Poor | Probably Inadequate | Adequate | Excellent | Usual food intake pattern |
| Friction & Shear | Problem | Potential Problem | No Apparent Problem | – | Degree of assistance required for moving and positioning |
Memory Aid: “SMAMF” for Braden Scale Domains
S – Sensory perception assessment
M – Moisture level evaluation
A – Activity level measurement
M – Mobility and positioning ability
F – Friction and shear risk factors
Plus: Nutrition status assessment
Norton Scale Assessment
The Norton Scale, developed by Doreen Norton in 1962, represents the pioneering pressure injury risk assessment tool that laid the foundation for modern pressure point care protocols. This streamlined assessment focuses on five key domains that significantly impact patient vulnerability to pressure injuries.
Historical Significance
- Year Developed: 1962
- Developer: Doreen Norton, RN
- Original Purpose: Geriatric care assessment
- Score Range: 5-20 points
- Assessment Time: 3-5 minutes
- Legacy: First standardized pressure injury risk tool
Norton Risk Categories
High Risk: ≤11 points
Immediate intervention required
Medium Risk: 12-14 points
Enhanced monitoring needed
Low Risk: ≥15 points
Standard care protocols
Complete Norton Scale Assessment Matrix
| Domain | 1 Point | 2 Points | 3 Points | 4 Points | Assessment Focus |
|---|---|---|---|---|---|
| Physical Condition | Very Bad | Poor | Fair | Good | General health status and vitality |
| Mental Condition | Stuporous | Confused | Apathetic | Alert | Cognitive function and awareness |
| Activity | Bedfast | Chairfast | Walks with Help | Ambulatory | Degree of physical mobility |
| Mobility | Immobile | Very Limited | Slightly Limited | Full | Ability to change position independently |
| Incontinence | Doubly Incontinent | Usually Incontinent | Occasionally Incontinent | Not Incontinent | Bladder and bowel control status |
Braden vs Norton Scale Comparison
| Aspect | Braden | Norton |
|---|---|---|
| Domains | 6 | 5 |
| Score Range | 6-23 | 5-20 |
| Specificity | Higher | Moderate |
| Best Use | Acute care | Long-term care |
Memory Aid: “PMAI” for Norton Scale
P – Physical condition assessment
M – Mental condition evaluation
A – Activity level measurement
I – Incontinence status check
Plus: Mobility assessment
Evidence-Based Prevention Strategies
Prevention remains the cornerstone of effective pressure point care, with evidence demonstrating that 95% of pressure injuries can be prevented through systematic implementation of evidence-based strategies. Comprehensive prevention programs integrate multiple interventions to address all risk factors simultaneously.
Repositioning Protocols
- • Frequency: Every 2 hours for bedbound patients
- • Chair positioning: Every 15 minutes or hourly
- • 30-degree rule: Avoid direct pressure on bony prominences
- • Pillow support: Use between bony prominences
- • Head elevation: Limit to 30 degrees maximum
- • Heel elevation: Float heels off bed surface
Support Surfaces
- • Foam mattresses: Basic pressure redistribution
- • Air-filled surfaces: Dynamic pressure relief
- • Low-air-loss beds: Moisture control features
- • Alternating pressure: Cyclical pressure relief
- • Gel overlays: Pressure distribution enhancement
- • Seat cushions: Wheelchair and chair protection
Skin Care Protocols
- • Daily inspection: Systematic skin assessment
- • Gentle cleansing: pH-balanced products
- • Moisturization: Maintain skin integrity
- • Barrier protection: Prevent moisture damage
- • Massaging contraindication: Avoid over bony prominences
- • Temperature monitoring: Check for skin changes
Critical Prevention Principles
The “Bundle” Approach:
- • Risk assessment standardization
- • Skin inspection protocols
- • Repositioning schedules
- • Nutritional optimization
- • Support surface selection
- • Staff education programs
Implementation Success Factors:
- • Leadership commitment
- • Interdisciplinary collaboration
- • Resource allocation
- • Performance monitoring
- • Continuous quality improvement
- • Patient and family engagement
Nutritional Considerations
Optimal nutrition supports pressure point care through:
- • Protein: 1.2-1.5g/kg body weight daily
- • Calories: 30-35 kcal/kg body weight
- • Vitamin C: 100-1000mg daily for healing
- • Zinc: 15-30mg daily for tissue repair
- • Hydration: 30ml/kg body weight minimum
Timing and Frequency Guidelines
| Intervention | Frequency |
|---|---|
| Risk assessment | Every 24-48 hours |
| Skin inspection | Daily minimum |
| Repositioning | Every 2 hours |
| Heel elevation | Continuous |
| Nutrition screening | Weekly |
Comprehensive Nursing Interventions
Effective pressure point care requires systematic implementation of evidence-based nursing interventions tailored to individual patient risk levels. These interventions encompass immediate protective measures, ongoing monitoring protocols, and collaborative care strategies that address the multifaceted nature of pressure injury prevention.
Immediate Interventions
High-Risk Patients (≤12 Braden Score):
- • Implement strict 2-hour repositioning schedule
- • Use specialized pressure-redistributing surfaces
- • Elevate heels completely off bed surface
- • Apply protective foam or gel pads
- • Initiate nutritional consultation
- • Implement moisture management protocols
Moderate-Risk Patients (13-14 Braden Score):
- • Establish regular repositioning schedule
- • Use pressure-reducing mattress overlay
- • Monitor skin condition twice daily
- • Implement preventive skin care measures
- • Encourage mobility and activity
- • Provide patient education on pressure point care
Ongoing Monitoring
Daily Assessment Protocol:
- • Systematic skin inspection during routine care
- • Temperature and texture changes documentation
- • Blanching response testing
- • Pain assessment at pressure points
- • Mobility and activity level evaluation
- • Nutritional and hydration status review
Documentation Requirements:
- • Risk scale scores with rationale
- • Detailed skin condition descriptions
- • Intervention implementation records
- • Patient response to interventions
- • Changes in risk factors or status
- • Interdisciplinary communication notes
Memory Aid: “INSPECT” Intervention Framework
I – Identify high-risk patients
N – Nutrition optimization
S – Skin assessment and care
P – Positioning and repositioning
E – Equipment and surface selection
C – Comfort and pain management
T – Teaching and education
Critical Intervention Mistakes to Avoid
- • Donut cushions: Increase pressure around wound edges
- • Massaging bony prominences: May cause tissue damage
- • Heat application: Increases metabolic demands
- • Inconsistent repositioning: Defeats prevention efforts
- • Ignoring early signs: Delays intervention
- • Inadequate documentation: Compromises continuity
Interdisciplinary Collaboration
Effective pressure point care requires coordination with:
- • Physicians: Medical management and orders
- • Dietitians: Nutritional assessment and planning
- • Physical therapists: Mobility and positioning
- • Occupational therapists: Adaptive equipment
- • Wound care specialists: Advanced treatment options
- • Family members: Education and support
Positioning and Offloading Techniques
Proper positioning and offloading techniques form the cornerstone of pressure point care, directly addressing the primary causative factor of pressure injuries. These evidence-based methods redistribute pressure, reduce shear forces, and maintain tissue perfusion while promoting patient comfort and mobility.
Bed Positioning Techniques
Supine Position (30-Degree Elevation):
- • Place pillow under head and shoulders
- • Support both arms with pillows
- • Position pillow under calves to elevate heels
- • Use small pillow for lumbar support
- • Avoid pressure on occiput, sacrum, and heels
Lateral Position (30-Degree Tilt):
- • Tilt patient to 30-degree angle
- • Place pillow behind back for support
- • Position pillow between legs
- • Support upper arm with pillow
- • Avoid direct pressure on greater trochanter
Chair Positioning Guidelines
Wheelchair Positioning:
- • Use appropriate pressure-redistribution cushion
- • Ensure proper seat depth and width
- • Position feet flat on footrests
- • Maintain upright posture with back support
- • Implement weight shifts every 15 minutes
Chair Transfer Techniques:
- • Limit sitting time to 2 hours maximum
- • Use proper body mechanics for transfers
- • Assess skin condition before and after sitting
- • Encourage active repositioning when possible
- • Monitor for signs of pressure intolerance
Repositioning Schedule Matrix
| Time | Position | Focus Areas |
|---|---|---|
| 8:00 AM | Supine | Heel elevation |
| 10:00 AM | Right lateral | Trochanter protection |
| 12:00 PM | Supine | Sacral offloading |
| 2:00 PM | Left lateral | Pressure redistribution |
Key Positioning Principles:
- • Maintain natural body alignment
- • Distribute weight evenly across surfaces
- • Avoid prolonged pressure on bony prominences
- • Use bridging techniques for wound protection
- • Ensure patient comfort throughout positioning
Offloading Equipment Selection
| Equipment | Indication | Effectiveness |
|---|---|---|
| Heel boots | Heel protection | High |
| Foam wedges | Positioning support | Moderate |
| Pressure pads | Bony prominence protection | High |
| Gel cushions | Pressure redistribution | Moderate |
Positioning Contraindications
- • 90-degree side-lying: Increases trochanter pressure
- • High head elevation: Increases sacral shear forces
- • Prone positioning: Limited use in acute care
- • Tight positioning: Restricts circulation
- • Ignoring patient comfort: Reduces compliance
Documentation and Monitoring Protocols
Comprehensive documentation and systematic monitoring are essential components of pressure point care that ensure continuity of care, legal protection, and quality improvement. Accurate record-keeping facilitates communication between healthcare team members and provides crucial data for evaluating intervention effectiveness.
Essential Documentation Elements
Risk Assessment Documentation:
- • Complete Braden or Norton scale scores
- • Rationale for individual domain scores
- • Date and time of assessment
- • Assessor identification and credentials
- • Changes from previous assessments
- • Reassessment schedule planning
Skin Assessment Records:
- • Detailed skin condition descriptions
- • Location-specific findings
- • Size, color, and texture changes
- • Blanching response results
- • Pain or discomfort levels
- • Photographic documentation when indicated
Monitoring Frequencies
Assessment Intervals:
- • High risk: Every 24 hours
- • Moderate risk: Every 48 hours
- • Low risk: Every 72 hours
- • Status change: Immediate reassessment
- • Admission: Within 8 hours
- • Transfer: Within 24 hours
Intervention Monitoring:
- • Repositioning schedule adherence
- • Support surface effectiveness
- • Skin care protocol compliance
- • Nutritional intervention outcomes
- • Patient tolerance and comfort
- • Family education and involvement
Legal and Regulatory Requirements
Required Documentation:
- • Risk assessment completion
- • Preventive intervention implementation
- • Patient and family education
- • Interdisciplinary communication
- • Incident reporting when applicable
- • Quality improvement participation
Regulatory Standards:
- • Joint Commission requirements
- • CMS quality reporting measures
- • State nursing practice standards
- • Facility policy compliance
- • Professional liability protection
- • Quality assurance protocols
Documentation Best Practices
- • Use objective, descriptive language
- • Include specific measurements and locations
- • Document in real-time when possible
- • Ensure legibility and completeness
- • Follow facility-specific guidelines
- • Include patient response to interventions
- • Maintain confidentiality and privacy
Quality Improvement Metrics
| Metric | Target | Frequency |
|---|---|---|
| Pressure injury rate | <2% | Monthly |
| Assessment compliance | 95% | Weekly |
| Intervention adherence | 90% | Daily |
| Staff competency | 100% | Annually |
Global Best Practices in Pressure Point Care
International healthcare organizations have developed innovative approaches to pressure point care that demonstrate significant improvements in patient outcomes and cost reduction. These evidence-based practices from around the world offer valuable insights for enhancing local care delivery and prevention programs.
United States Innovations
AHRQ Pressure Injury Prevention Program:
- • Comprehensive toolkit implementation
- • Evidence-based bundle approach
- • National data collection and benchmarking
- • Interdisciplinary team training programs
- • Results: 70% reduction in facility-acquired pressure injuries
Mayo Clinic SKIN Bundle:
- • S – Surface selection and optimization
- • K – Keep turning and repositioning
- • I – Incontinence and moisture management
- • N – Nutrition and hydration support
- • Outcome: 50% reduction in pressure injuries
United Kingdom Initiatives
NHS Safety Thermometer:
- • Monthly prevalence measurement system
- • Real-time data collection and analysis
- • National benchmarking and comparison
- • Quality improvement driver identification
- • Achievement: 23% reduction in pressure damage
SSKIN Care Bundle:
- • S – Surface assessment and selection
- • S – Skin assessment and care
- • K – Keep moving and positioning
- • I – Incontinence management
- • N – Nutrition and hydration
Australian “Pressure Injury Prevention” Model
The Australian Commission on Safety and Quality in Health Care developed a comprehensive pressure injury prevention model that achieved remarkable results across multiple healthcare settings.
Key Components:
- • National safety and quality standards
- • Mandatory pressure injury reporting
- • Standardized risk assessment protocols
- • Consumer and family engagement
- • Continuous professional development
Outcomes Achieved:
- • 40% reduction in hospital-acquired pressure injuries
- • $100 million annual cost savings
- • 95% compliance with prevention protocols
- • Enhanced patient satisfaction scores
- • Improved staff confidence and competency
Canadian “Safer Healthcare Now!” Campaign
Canada’s national patient safety initiative focused on pressure injury prevention through systematic implementation and measurement.
- • Approach: Plan-Do-Study-Act cycles
- • Focus: High-risk patient identification
- • Tools: Standardized assessment forms
- • Results: 60% reduction in pressure injuries
- • Sustainability: Embedded in quality programs
Scandinavian Technology Integration
Nordic countries have pioneered the integration of technology with pressure point care protocols.
- • Smart mattresses: Automated pressure redistribution
- • Sensor technology: Real-time positioning alerts
- • Mobile applications: Assessment and documentation
- • Predictive analytics: Risk identification algorithms
- • Results: 80% reduction in severe pressure injuries
Conclusion and Key Takeaways
Effective pressure point care represents a fundamental nursing competency that directly impacts patient outcomes, healthcare costs, and professional practice standards. Through systematic implementation of evidence-based assessment tools like the Braden and Norton scales, coupled with comprehensive prevention strategies, nursing professionals can significantly reduce pressure injury incidence and improve patient quality of life.
Essential Learning Points
Assessment Mastery:
- • Systematic risk assessment using validated tools
- • Comprehensive skin examination techniques
- • Recognition of early warning signs
- • Documentation accuracy and completeness
Prevention Excellence:
- • Evidence-based intervention implementation
- • Proper positioning and repositioning techniques
- • Appropriate support surface selection
- • Holistic patient care approach
Professional Development
Continued Learning:
- • Stay current with research and guidelines
- • Participate in professional development programs
- • Engage in quality improvement initiatives
- • Collaborate with interdisciplinary teams
Leadership Opportunities:
- • Champion best practices in clinical settings
- • Mentor junior nursing staff
- • Participate in policy development
- • Advocate for patient safety initiatives
The Impact of Excellence in Pressure Point Care
When nursing professionals master pressure point care, the ripple effects extend far beyond individual patient outcomes. Excellence in this fundamental area contributes to:
Patient Benefits:
- • Improved comfort and quality of life
- • Reduced length of stay
- • Decreased complications and mortality
- • Enhanced recovery outcomes
- • Preserved dignity and autonomy
Healthcare System Benefits:
- • Significant cost savings
- • Improved quality metrics
- • Enhanced reputation and accreditation
- • Reduced legal liability
- • Increased staff satisfaction
Final Memory Aid: “EXCELLENCE” in Pressure Point Care
E – Evaluate risk systematically
X – eXamine skin integrity daily
C – Collaborate with the healthcare team
E – Educate patients and families
L – Lead by example in practice
L – Learn continuously from evidence
E – Engage in quality improvement
N – Never compromise on safety
C – Care with compassion always
E – Ensure documentation accuracy
Your Journey Forward
As you continue your nursing career, remember that mastery of pressure point care is not a destination but a continuous journey of learning, improving, and caring. Each patient interaction provides an opportunity to apply these principles and make a meaningful difference in someone’s life.
Challenge yourself to: Implement one new evidence-based practice each month, mentor a colleague in pressure point care techniques, and advocate for resources that support optimal patient outcomes. Your commitment to excellence in this fundamental area of nursing will contribute to the advancement of our profession and the improvement of patient care worldwide.
