Nursing Care for Pressure Ulcers
Understanding Causes, Stages, Manifestations, and Prevention
Table of Contents
Introduction to Pressure Ulcers
Key Learning Objective
Understanding pressure ulcers is fundamental to nursing practice as they represent one of the most preventable healthcare complications, affecting millions of patients worldwide and significantly impacting quality of life.
Pressure ulcers, also known as bedsores or decubitus ulcers, are localized injuries to the skin and underlying tissues that result from prolonged pressure, friction, or shear forces. These injuries primarily occur over bony prominences and represent a significant healthcare challenge, affecting approximately 2.5 million patients annually in the United States alone.
The development of pressure ulcers involves complex pathophysiological processes that nurses must understand to provide effective care. When external pressure exceeds capillary perfusion pressure (typically 32 mmHg), tissue ischemia occurs, leading to cellular hypoxia and eventual tissue death if pressure is not relieved.
Clinical Significance
- • Healthcare-associated infections increase by 50% with pressure ulcers
- • Average treatment cost ranges from $500 to $70,000 per ulcer
- • Mortality rates increase by 2.8 times in patients with pressure ulcers
- • Hospital stays extend by an average of 4.31 days
Prevalence Statistics
- • Acute care: 8-12% of patients
- • Long-term care: 15-25% of residents
- • Home care: 17% of patients
- • ICU settings: Up to 40% of patients
Timeline of Development
- • Stage 1: 1-6 hours of pressure
- • Stage 2: 6-24 hours of pressure
- • Stage 3: 1-5 days of pressure
- • Stage 4: 5+ days of pressure
Causes and Risk Factors
Mnemonic: “PRESSURE” for Risk Factors
P – Prolonged immobility
R – Reduced sensation
E – Excessive moisture
S – Skin fragility
S – Shear and friction forces
U – Undernutrition
R – Reduced perfusion
E – Elderly population
Primary Causes
Pressure
Sustained compression of tissues between bony prominences and external surfaces, compromising blood flow and oxygen delivery.
Shear
Parallel forces causing tissue layers to slide against each other, typically occurring when patients slide down in bed.
Friction
Resistance to motion between skin and contact surfaces, particularly problematic during patient repositioning.
Comprehensive Risk Assessment
| Risk Category | Specific Factors | Mechanism | Nursing Implications |
|---|---|---|---|
| Mobility Impairment | Paralysis, sedation, cognitive impairment, musculoskeletal disorders | Inability to relieve pressure independently | Implement turning schedules, use pressure-redistributing devices |
| Sensory Impairment | Spinal cord injury, neuropathy, medication effects | Lack of awareness of pressure or discomfort | Educate on skin inspection, provide sensory substitutes |
| Nutritional Deficiency | Protein malnutrition, dehydration, vitamin deficiencies | Compromised tissue integrity and healing capacity | Nutritional assessment, dietary supplements, hydration management |
| Circulatory Compromise | Hypotension, anemia, peripheral vascular disease | Reduced tissue perfusion and oxygen delivery | Monitor vital signs, optimize circulation, positioning |
| Skin Moisture | Incontinence, perspiration, wound drainage | Maceration and weakening of skin barrier | Moisture management, barrier products, frequent cleansing |
High-Risk Populations
Medical Conditions
- • Diabetes mellitus
- • Cardiovascular disease
- • Kidney disease
- • Cerebrovascular accidents
Patient Populations
- • Elderly patients (>65 years)
- • ICU patients
- • Surgical patients
- • Patients with spinal cord injuries
Stages and Classifications
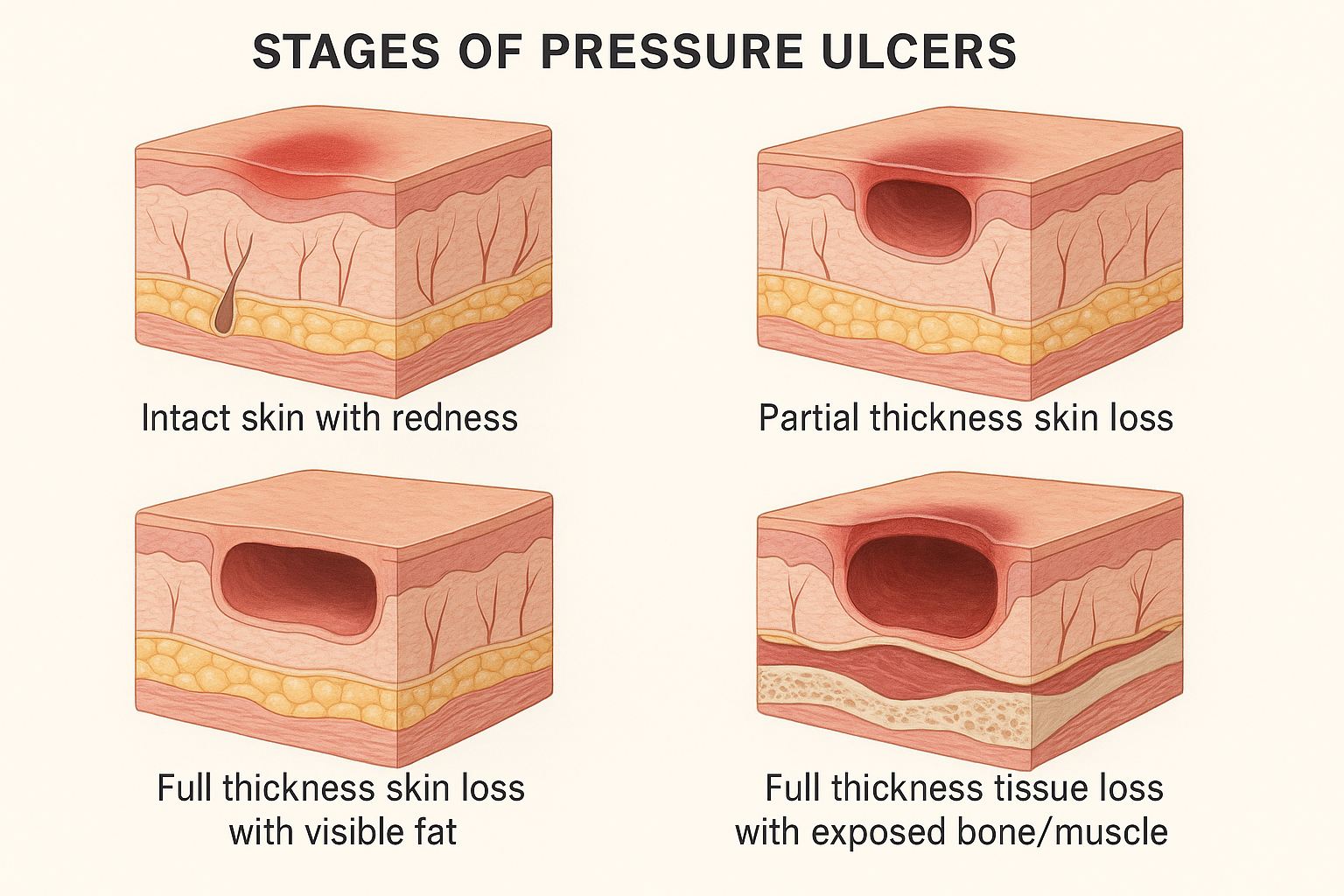
The National Pressure Ulcer Advisory Panel (NPUAP) classification system provides a standardized approach to categorizing pressure ulcers based on the depth of tissue involvement. Understanding these stages is crucial for nursing assessment and treatment planning.
Stage 1: Non-Blanchable Erythema
Appearance: Intact skin with localized area of non-blanchable erythema
Characteristics: May appear darker in darkly pigmented skin
Symptoms: Warmth, edema, induration, or hardness
Reversibility: Fully reversible with pressure relief
Stage 2: Partial Thickness Loss
Appearance: Partial thickness loss of dermis
Characteristics: Shallow open ulcer with red/pink wound bed
Symptoms: May present as intact or ruptured serum-filled blister
Healing time: 3-21 days with proper treatment
Stage 3: Full Thickness Loss
Appearance: Full thickness tissue loss with visible fat
Characteristics: Subcutaneous fat may be visible but not bone, tendon, or muscle
Symptoms: Slough may be present, undermining possible
Healing time: 1-6 months depending on size and location
Stage 4: Full Thickness Loss with Exposed Structures
Appearance: Full thickness tissue loss with exposed bone, tendon, or muscle
Characteristics: Slough or eschar may be present
Symptoms: Often includes undermining and tunneling
Healing time: 3 months to 2+ years, may require surgical intervention
Additional Classifications
Unstageable
Full thickness tissue loss where the base of the ulcer is covered by slough and/or eschar in the wound bed, making depth assessment impossible.
Suspected Deep Tissue Injury
Purple or maroon localized area of discolored intact skin or blood-filled blister due to damage of underlying soft tissue from pressure and/or shear.
Mnemonic: “SKIN” for Stage Assessment
S – Surface integrity (intact vs. broken)
K – Knowledge of tissue layers involved
I – Identify depth of tissue loss
N – Note presence of slough or eschar
Assessment Tools and Techniques
The Braden Scale: Gold Standard Assessment
The Braden Scale is the most widely used tool for assessing pressure ulcer risk, evaluating six key factors with scores ranging from 6-23, where lower scores indicate higher risk.
| Braden Scale Component | Score Range | Assessment Criteria | Nursing Considerations |
|---|---|---|---|
| Sensory Perception | 1-4 | Ability to respond meaningfully to pressure-related discomfort | Assess cognitive function, pain perception, consciousness level |
| Moisture | 1-4 | Degree to which skin is exposed to moisture | Evaluate incontinence, perspiration, drainage |
| Activity | 1-4 | Degree of physical activity | Assess mobility limitations, bedrest requirements |
| Mobility | 1-4 | Ability to change and control body position | Evaluate range of motion, turning ability |
| Nutrition | 1-4 | Usual food intake pattern | Assess dietary intake, albumin levels, weight changes |
| Friction and Shear | 1-3 | Degree of assistance needed for movement | Evaluate sliding, repositioning needs |
19-23 Points
LOW RISK
Minimal intervention needed
15-18 Points
MODERATE RISK
Preventive measures indicated
13-14 Points
HIGH RISK
Aggressive prevention needed
≤12 Points
VERY HIGH RISK
Immediate intensive interventions required
Comprehensive Skin Assessment
OBSERVE Assessment Framework
O – Observe skin color and temperature
B – Blanch test for capillary refill
S – Skin integrity and moisture
E – Edema and induration
R – Range of motion assessment
V – Vital signs and circulation
E – Evaluate pain and sensation
Assessment Frequency
- • High risk patients: Every 8 hours
- • Moderate risk patients: Every 12 hours
- • Low risk patients: Every 24 hours
- • ICU patients: Every 4-6 hours
- • Post-operative patients: Every 2-4 hours
High-Risk Body Areas
- • Sacrum and coccyx
- • Heels and ankles
- • Hips and trochanters
- • Elbows and shoulder blades
- • Back of head (in infants)
Red Flag Indicators
Immediate nursing intervention required when observing: non-blanchable erythema, skin temperature changes, new areas of discoloration, patient reports of pain or discomfort over bony prominences, or any signs of tissue breakdown.
Prevention Strategies
Prevention is Key
Research shows that 95% of pressure ulcers are preventable through proper nursing interventions. The key is implementing evidence-based prevention strategies consistently and systematically.
Mnemonic: “PREVENT” for Prevention Strategies
P – Position changes every 2 hours
R – Reduce pressure with devices
E – Educate patient and family
V – Vigilant skin assessment
E – Ensure proper nutrition
N – Nutrition and hydration
T – Turn and reposition regularly
Core Prevention Interventions
Repositioning and Mobility
- • Turn every 2 hours for bedridden patients
- • Use 30-degree lateral positioning
- • Avoid direct pressure on bony prominences
- • Encourage small shifts in weight every 15 minutes
- • Implement progressive mobility protocols
- • Use proper body mechanics during transfers
Support Surfaces
- • Static air mattresses for moderate risk
- • Alternating pressure mattresses for high risk
- • Foam overlays for low-risk patients
- • Gel cushions for wheelchair users
- • Heel protectors and elbow guards
- • Avoid donut-shaped cushions
| Prevention Strategy | Implementation | Frequency | Expected Outcome |
|---|---|---|---|
| Skin Care | Gentle cleansing, moisturizing, barrier protection | Daily or as needed | Maintain skin integrity, prevent breakdown |
| Nutrition Support | Protein supplementation, adequate hydration | Continuous | Promote tissue healing, maintain skin health |
| Moisture Management | Incontinence care, absorbent products | As needed | Prevent skin maceration, maintain dry environment |
| Pressure Relief | Positioning devices, support surfaces | Every 2 hours | Reduce prolonged pressure, improve circulation |
Specialized Prevention Protocols
Nutritional Support
- • Protein: 1.2-1.5 g/kg/day
- • Calories: 30-35 kcal/kg/day
- • Vitamin C: 500-1000 mg/day
- • Zinc: 15-30 mg/day
- • Fluid: 30-35 ml/kg/day
Moisture Control
- • Use pH-balanced cleansers
- • Apply moisture barriers
- • Change incontinence products promptly
- • Use absorbent underpads
- • Maintain room humidity 40-60%
Turning Schedule
- • Every 2 hours for bed patients
- • Every 1 hour for chair patients
- • Use turning clocks/charts
- • Document position changes
- • Adjust based on risk level
Family and Patient Education
Educate patients and families about risk factors, prevention strategies, and the importance of regular position changes. Provide written materials and demonstrations of proper positioning techniques. Encourage active participation in prevention activities when possible.
Management and Treatment
Treatment Goals
Treatment of pressure ulcers focuses on creating optimal conditions for healing while preventing further tissue damage. The approach must be individualized based on ulcer stage, patient condition, and available resources.
Mnemonic: “HEALING” for Treatment Approach
H – Hydration and nutrition
E – Eliminate pressure sources
A – Assess and clean wound
L – Local wound care
I – Infection prevention
N – Nutrition optimization
G – Growth factor support
Stage-Specific Treatment Protocols
Stage 1 & 2 Treatment
- • Transparent film dressings
- • Hydrocolloid dressings
- • Foam dressings for moderate exudate
- • Gentle cleansing with normal saline
- • Moisture balance maintenance
- • Continue pressure relief measures
Stage 3 & 4 Treatment
- • Debridement (surgical, mechanical, enzymatic)
- • Alginate dressings for heavy exudate
- • Negative pressure wound therapy
- • Antimicrobial dressings if infected
- • Surgical consultation for severe cases
- • Nutritional support intensification
| Wound Assessment Parameter | Normal/Healthy | Concerning Signs | Nursing Action |
|---|---|---|---|
| Wound Bed | Pink to red, granulation tissue | Black eschar, yellow slough | Prepare for debridement, consider enzymatic agents |
| Exudate | Minimal, clear to light yellow | Purulent, malodorous, excessive | Culture wound, notify physician, antimicrobial therapy |
| Wound Edges | Pink, attached, epithelializing | Rolled, undermined, necrotic | Assess for infection, consider advanced therapies |
| Periwound Skin | Intact, normal color | Macerated, inflamed, indurated | Improve moisture management, barrier protection |
Advanced Treatment Modalities
Negative Pressure Wound Therapy
- • Promotes granulation tissue
- • Reduces edema
- • Removes excess exudate
- • Increases blood flow
- • Accelerates healing
Bioengineered Therapies
- • Growth factor therapies
- • Platelet-derived products
- • Tissue-engineered skin
- • Stem cell therapies
- • Hyperbaric oxygen therapy
Surgical Interventions
- • Surgical debridement
- • Flap reconstruction
- • Skin grafting
- • Myocutaneous flaps
- • Hardware removal
Infection Management
Signs of infection include increased pain, erythema, warmth, swelling, purulent drainage, and systemic symptoms. Immediate intervention required for:
- • Wound cultures and sensitivity testing
- • Antimicrobial therapy (topical or systemic)
- • Enhanced wound cleansing protocols
- • Isolation precautions if indicated
Monitoring Treatment Progress
Document wound measurements, photographs, and healing progress weekly. Expect 20-40% reduction in wound size every 2-4 weeks with appropriate treatment. Reassess treatment plan if no improvement after 2 weeks or if wound deteriorates.
Patient Education
Education Empowers Prevention
Effective patient education is crucial for preventing pressure ulcers and promoting healing. Patients and families who understand the risks and prevention strategies are more likely to actively participate in care and achieve better outcomes.
Mnemonic: “TEACH” for Patient Education
T – Tell them about pressure ulcers
E – Explain risk factors and prevention
A – Assess their understanding
C – Clarify misconceptions
H – Help them develop care plan
Core Educational Topics
Understanding Pressure Ulcers
- • What are pressure ulcers and how they develop
- • Risk factors specific to patient’s condition
- • Signs and symptoms to watch for
- • Importance of early detection
- • Impact on health and quality of life
- • Preventability with proper care
Prevention Strategies
- • Proper positioning techniques
- • Importance of movement and repositioning
- • Skin inspection methods
- • Nutritional requirements
- • Moisture management
- • Equipment use and care
| Education Topic | Key Messages | Teaching Methods | Evaluation |
|---|---|---|---|
| Skin Inspection | Daily inspection, use of mirrors, recognition of warning signs | Demonstration, return demonstration, written guides | Patient demonstrates technique correctly |
| Positioning | Every 2 hours, avoid pressure points, use of pillows | Hands-on practice, positioning aids, timers | Family members position patient correctly |
| Nutrition | Protein intake, hydration, supplements | Dietary consultation, meal planning, supplements | Patient maintains adequate nutritional intake |
| Equipment Use | Proper use of cushions, mattresses, heel protectors | Equipment demonstration, fitting, maintenance | Correct equipment use at home |
Special Populations Education
Spinal Cord Injury
- • Weight shifting techniques
- • Pressure mapping
- • Wheelchair cushion selection
- • Transfer techniques
- • Lifetime prevention strategies
Family Caregivers
- • Caregiver safety techniques
- • Recognizing caregiver fatigue
- • Community resources
- • Equipment maintenance
- • Emergency procedures
Home Care Patients
- • Environmental modifications
- • Supply management
- • When to call healthcare provider
- • Documentation methods
- • Insurance considerations
Patient Education Checklist
Before Discharge:
- ☐ Skin inspection technique demonstrated
- ☐ Positioning schedule established
- ☐ Equipment properly fitted
- ☐ Nutrition plan reviewed
Follow-up Required:
- ☐ Equipment function assessed
- ☐ Caregiver competency verified
- ☐ Questions and concerns addressed
- ☐ Community resources connected
When to Contact Healthcare Provider
Educate patients to contact healthcare providers immediately if they notice:
- • New areas of redness that don’t blanch
- • Any open wounds or blisters
- • Signs of infection (fever, increased pain, drainage)
- • Changes in existing wounds
- • Equipment malfunction or discomfort
Global Best Practices
International Excellence in Pressure Ulcer Prevention
Healthcare systems worldwide have developed innovative approaches to pressure ulcer prevention, achieving remarkable reductions in incidence rates through evidence-based practices and quality improvement initiatives.
Netherlands: “Zero Tolerance” Initiative
- • Implemented national “zero tolerance” policy
- • Achieved 50% reduction in pressure ulcer incidence
- • Mandatory risk assessment within 6 hours
- • Standardized prevention protocols
- • Quality indicators tied to hospital funding
- • Multidisciplinary team approach
Canada: “Safer Healthcare Now!”
- • National patient safety campaign
- • Reduced pressure ulcer rates by 25%
- • Standardized assessment tools
- • Best practice guidelines implementation
- • Continuous quality improvement
- • Patient and family engagement
| Country/Region | Initiative | Key Strategies | Results Achieved |
|---|---|---|---|
| Australia | National Safety and Quality Health Service Standards | Mandatory reporting, standardized protocols, staff education | 30% reduction in hospital-acquired pressure ulcers |
| United Kingdom | NHS Stop the Pressure Programme | React to red campaign, SSKIN bundle, collaborative learning | 23% reduction in pressure ulcer incidence |
| Germany | Dekubitus Network | Evidence-based guidelines, certification program, quality indicators | Improved compliance with prevention measures |
| Japan | Pressure Ulcer Prevention Society | National guidelines, education programs, research promotion | Enhanced awareness and prevention practices |
Innovative Prevention Technologies
Smart Monitoring Systems
- • Sensor-based pressure monitoring
- • Automated turning reminders
- • Real-time risk assessment
- • Predictive analytics
- • Mobile health applications
Robotic Assistance
- • Automated patient turning systems
- • Robotic lifting devices
- • Pressure redistribution beds
- • AI-powered risk assessment
- • Telemedicine monitoring
Advanced Materials
- • Temperature-regulating fabrics
- • Pressure-mapping textiles
- • Antimicrobial surfaces
- • Shape-memory foam
- • Moisture-wicking materials
Key Success Factors from Global Initiatives
- • Leadership commitment and organizational culture change
- • Standardized, evidence-based protocols
- • Comprehensive staff education and training
- • Patient and family engagement
- • Continuous monitoring and quality improvement
- • Multidisciplinary collaboration
- • Technology integration and innovation
Future Directions
The future of pressure ulcer prevention lies in personalized medicine approaches, artificial intelligence-driven risk prediction, advanced biomaterials, and integrated care models that span acute, long-term, and home care settings. These innovations, combined with continued focus on education and quality improvement, promise to make pressure ulcers a truly preventable condition.
Conclusion
Nursing Excellence in Pressure Ulcer Care
Pressure ulcers represent a significant challenge in healthcare, but they are largely preventable through evidence-based nursing interventions. As healthcare professionals, our commitment to excellence in pressure ulcer prevention and management directly impacts patient outcomes, quality of life, and healthcare costs.
The comprehensive approach to pressure ulcer care requires integration of assessment, prevention, treatment, and education strategies. By implementing systematic risk assessment using validated tools like the Braden Scale, maintaining vigilant skin monitoring, and ensuring appropriate prevention interventions, nurses can significantly reduce the incidence of pressure ulcers in their patient populations.
The evolution of pressure ulcer care continues with advancing technologies, improved understanding of wound healing physiology, and innovative treatment modalities. However, the foundation of successful pressure ulcer prevention remains rooted in fundamental nursing principles: thorough assessment, individualized care planning, patient education, and continuous quality improvement.
Key Takeaways
- • 95% of pressure ulcers are preventable
- • Early identification is crucial for prevention
- • Multidisciplinary approach improves outcomes
- • Patient education empowers self-care
- • Continuous assessment drives interventions
Next Steps
- • Implement standardized protocols
- • Enhance staff education programs
- • Integrate technology solutions
- • Strengthen quality improvement initiatives
- • Expand research and evidence base
Remember: Every Patient Deserves Skin Integrity
“Pressure ulcers are not just wounds – they represent opportunities for nursing excellence in prevention, early intervention, and compassionate care.”
