Common Behavioral Disorders in Children
Nursing Management of Enuresis and Encopresis
Table of Contents
- Introduction to Childhood Behavioral Disorders
- Common Behavioral Disorders in Children
- Enuresis: Overview and Diagnosis
- Encopresis: Overview and Diagnosis
- Nursing Assessment
- Nursing Management in Hospital Settings
- Home-Based Nursing Management
- Behavioral Management Techniques
- Mnemonics for Nursing Practice
- Case Studies
- Conclusion
- References
1. Introduction to Childhood Behavioral Disorders
Childhood behavioral disorders represent a significant challenge for healthcare providers, families, and the affected children themselves. These conditions can impact a child’s social, emotional, and educational development, making early identification and appropriate management crucial for optimal outcomes.
Definition: Behavioral disorders in children are characterized by a pattern of disruptive behaviors that last for at least 6 months and cause problems in school, at home, and in social situations. Unlike occasional behavioral issues that all children experience, these disorders involve persistent patterns that significantly impair functioning across multiple settings.
Among the various behavioral disorders that affect children, elimination disorders—specifically enuresis (involuntary urination) and encopresis (involuntary defecation)—represent common but often underaddressed conditions that can cause significant distress and social impairment for affected children and their families.
As nursing professionals, understanding the diagnostic criteria, assessment methods, and evidence-based management approaches for these conditions is essential for providing comprehensive care. Effective behavioral management requires a multidisciplinary approach that addresses the underlying physiological, psychological, and social factors contributing to these conditions.
Why These Notes Matter: These comprehensive notes aim to equip nursing students with the knowledge and clinical tools needed to provide evidence-based care for children with elimination disorders. By implementing effective behavioral management strategies, nurses can play a pivotal role in improving outcomes and quality of life for these children and their families.
2. Common Behavioral Disorders in Children
Before focusing specifically on elimination disorders, it’s important to understand the broader context of behavioral disorders in children. The most common disruptive behavioral disorders include:
| Disorder | Key Characteristics | Prevalence | Age of Onset |
|---|---|---|---|
| Attention Deficit Hyperactivity Disorder (ADHD) | Persistent pattern of inattention, hyperactivity, and impulsivity that interferes with functioning or development | 5-10% of school-aged children | Before age 12, often noticeable by age 6 |
| Oppositional Defiant Disorder (ODD) | Pattern of angry/irritable mood, argumentative/defiant behavior, or vindictiveness lasting at least 6 months | 2-16% of children | Usually before age 8 |
| Conduct Disorder (CD) | Persistent pattern of behavior that violates the rights of others or societal norms | 1-10% of children, more common in boys | Childhood onset: before age 10 Adolescent onset: after age 10 |
| Enuresis | Repeated involuntary or intentional urination in inappropriate places | 5-10% of 5-year-olds, 3-5% of 10-year-olds | After age 5 (when toilet training should be established) |
| Encopresis | Repeated passage of feces in inappropriate places | 1-3% of children aged 4-10 years | After age 4 (when toilet training should be established) |
While ADHD, ODD, and CD are often what come to mind when discussing behavioral disorders, elimination disorders like enuresis and encopresis represent a significant subset that requires specific nursing attention and behavioral management approaches.
Important Note: Boys are more likely than girls to experience behavioral disorders overall, including elimination disorders. Cultural factors, parenting styles, and environmental stressors can also influence the manifestation and management of these conditions.
Understanding the relationships between different behavioral disorders is crucial for comprehensive assessment and management. For instance, children with ADHD may have higher rates of enuresis due to delayed maturation of central nervous system functions. Similarly, children with encopresis may develop secondary behavioral problems related to social stigma and reduced self-esteem.
Effective behavioral management of elimination disorders requires a thorough understanding of the underlying physiological mechanisms, psychological factors, and environmental influences that contribute to these conditions.
3. Enuresis: Overview and Diagnosis
3.1 Definition and Types
Definition: Enuresis refers to the involuntary passage of urine in inappropriate places (e.g., clothing, bed) in a child who is developmentally expected to have achieved bladder control (typically age 5 or older).
Enuresis is classified based on two main factors:
Time of Occurrence:
- Nocturnal Enuresis: Occurs during sleep (bedwetting)
- Diurnal Enuresis: Occurs during waking hours
- Mixed Enuresis: Occurs during both sleep and waking hours
Etiology:
- Primary Enuresis: Child has never achieved a period of sustained dryness (at least 6 months)
- Secondary Enuresis: Child had achieved dryness for at least 6 months before the onset of wetting
3.2 Diagnostic Criteria
According to clinical guidelines, the diagnostic criteria for enuresis include:
- Chronological or developmental age of at least 5 years
- Repeated voiding of urine into bed or clothes (whether involuntary or intentional)
- Frequency of at least twice a week for three consecutive months
- The behavior is not due exclusively to the direct physiological effect of a substance or a general medical condition
Clinical Alert: Secondary enuresis warrants thorough investigation as it may indicate underlying medical conditions such as urinary tract infection, diabetes, sleep apnea, or neurological disorders. It can also be triggered by psychological stressors like family conflict, moving, or starting school.
3.3 Epidemiology and Risk Factors
Prevalence:
- 15% of children at age 5
- 7-10% of children at age 7
- 3-5% of children at age 10
- 1-2% of adolescents at age 15
- Boys are affected 1.5-2 times more frequently than girls
Risk Factors:
- Genetic predisposition (70-80% of children with enuresis have a first-degree relative with history of the condition)
- Developmental delays
- Sleep disorders (especially deep sleep)
- Neurological conditions
- Delayed bladder maturation
- Reduced nocturnal antidiuretic hormone (ADH) production
- Psychological stressors
- Constipation (can place pressure on the bladder)
3.4 Pathophysiology
Understanding the pathophysiology of enuresis is crucial for effective behavioral management. Three main mechanisms contribute to enuresis:
1. Nocturnal Polyuria
Excessive urine production during sleep due to:
- Decreased nocturnal ADH secretion
- Failure of normal circadian rhythm of ADH
- Increased evening fluid intake
2. Bladder Dysfunction
Problems with bladder function, including:
- Reduced functional bladder capacity
- Bladder overactivity
- Delayed maturation of bladder control
3. Sleep Arousal Dysfunction
Inability to wake in response to bladder signals due to:
- Abnormally deep sleep
- Deficient arousal response to bladder fullness
- Altered sleep architecture
Urinary System Anatomy
Source: Cincinnati Children’s Hospital
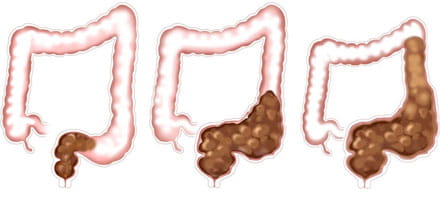
4. Encopresis: Overview and Diagnosis
4.1 Definition and Types
Definition: Encopresis refers to the repeated passage of feces in inappropriate places (e.g., clothing or floor) in a child who is developmentally expected to have achieved bowel control (typically age 4 or older).
Encopresis is classified based on etiology:
- Retentive Encopresis (95% of cases): Associated with constipation and fecal impaction
- Non-retentive Encopresis (5% of cases): Not associated with constipation, often related to psychological factors
Important Distinction: Understanding whether encopresis is retentive or non-retentive is crucial for appropriate behavioral management and treatment planning.
4.2 Diagnostic Criteria
According to clinical guidelines, the diagnostic criteria for encopresis include:
- Chronological or developmental age of at least 4 years
- Repeated passage of feces into inappropriate places (whether involuntary or intentional)
- Occurrence at least once per month for at least 3 consecutive months
- The behavior is not due exclusively to the direct physiological effect of a substance or a general medical condition except through a mechanism involving constipation
Clinical Presentation: Children with retentive encopresis often present with soiling, infrequent bowel movements, large-diameter stools, pain during defecation, and abdominal pain.
4.3 Epidemiology and Risk Factors
Prevalence:
- 1-3% of children aged 4-10 years
- Boys are affected 3-6 times more frequently than girls
- Peak incidence at 5-6 years of age
- Spontaneous resolution rate of 15% per year
Risk Factors:
- History of constipation
- Painful bowel movements leading to stool withholding
- Inadequate toilet training
- Dietary factors (low fiber, high dairy)
- Psychological stressors
- Family history of bowel problems
- Neurodevelopmental disorders
- Anatomical abnormalities (rare)
4.4 Pathophysiology of Retentive Encopresis
The pathophysiology of retentive encopresis typically follows a cyclical pattern:
Stage 1: Initial Constipation
Child experiences painful bowel movement due to constipation (often from dietary factors, illness, or disruption in routine)
Stage 2: Stool Withholding
Child begins to withhold stool to avoid discomfort, leading to harder stools and reinforcing the withholding behavior
Stage 3: Rectal Distention
Rectum becomes distended with accumulated stool, leading to decreased rectal tone and sensation
Stage 4: Impaction
Fecal impaction occurs, with hard stool mass in rectum
Stage 5: Overflow Incontinence
Liquid stool leaks around the impaction, causing involuntary soiling
Key Insight: In retentive encopresis, the soiling is often involuntary and occurs when liquid stool leaks around the impacted fecal mass. The child may not feel the leakage due to decreased rectal sensation from chronic distention. This is why punitive approaches are counterproductive and appropriate behavioral management is crucial.
5. Nursing Assessment
Comprehensive nursing assessment is the foundation for effective behavioral management of elimination disorders. Assessment should be thorough, culturally sensitive, and age-appropriate.
5.1 Assessment of Enuresis
Subjective Data Collection:
- Frequency of episodes (≥ twice weekly for 3 months for diagnosis)
- Timing of episodes (nocturnal, diurnal, or both)
- Duration of the problem
- Pattern (primary vs. secondary enuresis)
- Associated symptoms (dysuria, urgency, frequency, etc.)
- Age of toilet training
- Method of toilet training
- Previous periods of dryness
- Developmental milestones
- Amount and timing of fluid intake
- Types of beverages (caffeine, carbonated drinks)
Additional Assessment Areas:
- Impact on child’s self-esteem and social interactions
- Family response to episodes
- Recent life stressors or changes
- School performance and attendance
- Family history of enuresis
- Family history of urological or renal conditions
- Previous treatments and outcomes
- Current medications
- History of UTIs or renal conditions
- Neurological conditions
- Sleep patterns and disorders
Objective Assessment:
- Abdominal examination (palpable bladder, masses)
- Genital examination (abnormalities, signs of irritation)
- Lower back examination (signs of spina bifida occulta)
- Neurological assessment of lower extremities
- To rule out infection, diabetes, or other abnormalities
- Check for presence of blood, protein, glucose
- Assess urine concentration and specific gravity
- Frequency and timing of urination
- Voided volumes
- Fluid intake (timing, type, amount)
- Episodes of urgency, frequency, or incontinence
- Abdominal distention
- Palpable fecal masses
- Bowel movement frequency and characteristics
5.2 Assessment of Encopresis
Subjective Data Collection:
- Frequency of soiling episodes
- Duration of the problem
- Associated symptoms (abdominal pain, appetite changes)
- Bowel movement patterns (frequency, consistency, size)
- Pain or discomfort with defecation
- Fiber intake
- Fluid intake
- Dairy consumption
- Fast food frequency
Additional Assessment Areas:
- Age at toilet training
- Method of toilet training
- Child’s reaction to toilet training
- Previous success with bowel control
- Impact on child’s self-esteem
- School performance and attendance
- Peer relationships
- Family dynamics and response to soiling
- Recent life stressors or changes
Objective Assessment:
- Abdominal examination (distention, palpable fecal masses)
- Digital rectal examination (if indicated, to assess for impaction)
- Perianal inspection (fissures, hemorrhoids, inflammation)
- Assessment of anal tone and reflexes
- Growth parameters (height, weight, BMI)
- Frequency of bowel movements
- Stool consistency using Bristol Stool Chart
- Episodes of soiling
- Pain or straining with defecation
- Abdominal X-ray to assess for fecal loading
- Basic laboratory studies to rule out organic causes
- Signs of stool withholding (posturing, crossing legs)
- Toileting behaviors
- Response to soiling episodes
Assessment Tools: Using standardized assessment tools can enhance the comprehensive evaluation of elimination disorders. Consider using:
- Dysfunctional Voiding Symptom Score (DVSS) for enuresis
- Bristol Stool Form Scale for encopresis
- Pediatric Quality of Life Inventory (PedsQL) to assess psychosocial impact
6. Nursing Management in Hospital Settings
While most children with elimination disorders are managed on an outpatient basis, hospitalization may be necessary in certain circumstances such as severe constipation requiring manual disimpaction, concurrent medical conditions, or for intensive behavioral management programs. Nurses play a crucial role in the multidisciplinary hospital management of these conditions.
6.1 Hospital Management of Enuresis
Nursing Diagnosis:
- Functional Urinary Incontinence related to bladder dysfunction or developmental delay
- Disturbed Sleep Pattern related to enuresis episodes and treatment interventions
- Situational Low Self-Esteem related to lack of control over elimination
- Risk for Impaired Skin Integrity related to moisture from urine
- Deficient Knowledge regarding management of enuresis
Assessment in Hospital Setting:
- Continuous monitoring of voiding patterns
- Measurement of intake and output
- Urinalysis and urine culture
- Assessment of skin integrity in perineal area
- Evaluation of sleep patterns
- Psychological assessment
Nursing Interventions:
- Maintain accurate intake and output records
- Record frequency, timing, and circumstances of incontinence episodes
- Monitor response to interventions
- Implement scheduled voiding times (typically every 2-3 hours during daytime)
- Teach double voiding technique
- Provide positive reinforcement for successful toileting
- Maintain adequate hydration during daytime
- Limit fluid intake 2-3 hours before bedtime
- Avoid caffeine and carbonated beverages
- Desmopressin (DDAVP): Administer as ordered, typically before bedtime
- Anticholinergics: Monitor for side effects (dry mouth, constipation)
- Provide education about medication purpose, administration, and side effects
- Implement skin care protocol to prevent breakdown
- Change wet clothing and bedding promptly
- Teach proper hygiene to prevent complications
- Maintain a non-punitive, supportive approach
- Provide privacy during toileting and episodes
- Include child in management plan as appropriate for age
- Offer encouragement and positive reinforcement
- Develop comprehensive home management plan
- Educate about enuresis alarms if prescribed
- Provide resources for ongoing support
- Schedule follow-up appointments
6.2 Hospital Management of Encopresis
Nursing Diagnosis:
- Constipation related to inadequate fluid/fiber intake and stool withholding behavior
- Bowel Incontinence related to chronic constipation and rectal distention
- Situational Low Self-Esteem related to social implications of soiling
- Risk for Impaired Skin Integrity related to contact with fecal material
- Compromised Family Coping related to chronic nature of condition
Assessment in Hospital Setting:
- Abdominal assessment for distention and impaction
- Rectal examination (if indicated)
- Monitoring of bowel movements (frequency, consistency, amount)
- Dietary intake assessment
- Psychosocial assessment of child and family
Nursing Interventions:
- Administer oral laxatives as prescribed
- Provide enemas or suppositories as ordered
- Assist with manual disimpaction if required
- Monitor patient’s response and discomfort
- Administer maintenance laxatives as prescribed
- Implement bowel management protocol
- Maintain stool diary
- Monitor for effectiveness of interventions
- Collaborate with dietitian to increase fiber intake
- Encourage adequate fluid intake
- Limit constipating foods (excessive dairy, processed foods)
- Document dietary tolerance and response
- Implement regular toilet sitting times (usually after meals)
- Ensure proper positioning on toilet (feet supported, comfortable position)
- Provide privacy and adequate time
- Use positive reinforcement for cooperation
- Implement skin care protocol for perineal area
- Teach and assist with proper cleaning techniques
- Manage odor with appropriate interventions
- Ensure clean clothing is available
- Use non-punitive, matter-of-fact approach
- Educate about physiological basis of encopresis
- Involve child in age-appropriate management
- Provide emotional support to child and family
- Educate about behavioral management strategies
Hospital Discharge Planning: Preparation for discharge should begin early during hospitalization. Key components include:
- Comprehensive education on home management plan
- Ensuring family understands medication regimen
- Providing written instructions for bowel/bladder programs
- Connecting family with community resources
- Scheduling appropriate follow-up appointments
- Addressing school-related concerns
7. Home-Based Nursing Management
The majority of children with elimination disorders are managed in home settings. Nurses play a crucial role in developing, teaching, and monitoring home-based behavioral management programs. Successful management requires a collaborative approach involving the child, family, healthcare providers, and sometimes school personnel.
7.1 Home Management of Enuresis
Fluid Management:
Recommended Protocol:
- Ensure adequate hydration during daytime (70% of fluids before 5 PM)
- Limit fluids 2-3 hours before bedtime
- Avoid caffeine, carbonated beverages, and citrus juices
- Use a daily fluid intake record to monitor compliance
Voiding Schedule:
Structured Voiding Program:
- Regular voiding every 2-3 hours during daytime
- Double voiding before bedtime (void, wait 10 minutes, void again)
- Wake for scheduled voiding during night (initially)
- Gradually extend intervals between voidings
Bedwetting Alarms:
Implementation Guidelines:
- Select appropriate alarm type (body-worn or pad-type)
- Instruct on proper use and maintenance
- Establish routine for response to alarm
- Continue use for 2-3 months or until 14 consecutive dry nights
- Consider overlearning (increased fluid intake before bed) to prevent relapse
Reward Systems:
Effective Reinforcement:
- Implement star charts or token systems
- Reward effort and compliance, not just dry nights
- Set achievable goals with graduated rewards
- Avoid punishment for wet episodes
- Involve child in selecting rewards
Medication Management:
| Medication | Dosage | Administration | Nursing Considerations |
|---|---|---|---|
| Desmopressin (DDAVP) | 0.2-0.6 mg PO or 10-40 μg intranasal | One hour before bedtime |
|
| Anticholinergics (Oxybutynin) | 5-10 mg daily | Divided doses or extended-release |
|
| Imipramine | 25-50 mg for 7-10 years 50-75 mg for older children |
One hour before bedtime |
|
Practical Home Management Tips:
- Use waterproof mattress protectors
- Layer bedding for easy nighttime changes
- Have clean pajamas readily available
- Teach child to assist with changing (age-appropriate)
- Normalize the condition (emphasize prevalence)
- Maintain confidentiality outside family
- Provide age-appropriate explanation
- Focus on child’s strengths in other areas
- Ensure regular bathroom access during school hours
- Provide discrete plan for accidents at school
- Consider limiting school activities only if necessary
- Maintain voiding diary
- Track dry and wet nights
- Document response to interventions
- Regular follow-up with healthcare providers
7.2 Home Management of Encopresis
Successful home management of encopresis typically involves a multi-faceted approach addressing the physiological, behavioral, and psychosocial aspects of the condition. The core components include:
Phase 1
Disimpaction
- Oral laxatives as prescribed
- Enemas if needed (usually administered in clinical setting)
- Monitor bowel movements
- Adequate hydration
- May take 3-7 days
Phase 2
Prevention of Reaccumulation
- Maintenance laxatives
- High-fiber diet
- Regular toilet sitting schedule
- Adequate hydration
- May continue for 3-6 months
Phase 3
Behavioral Reconditioning
- Toilet sitting routine
- Positive reinforcement
- Gradual withdrawal of laxatives
- Ongoing monitoring
- May continue for 6-24 months
Medication Management:
| Medication Type | Examples | Purpose | Nursing Considerations |
|---|---|---|---|
| Osmotic Laxatives | Polyethylene glycol (PEG), Lactulose, Milk of Magnesia | Initial cleanout and maintenance |
|
| Stimulant Laxatives | Senna, Bisacodyl | Promote bowel motility |
|
| Stool Softeners | Docusate sodium | Soften stool consistency |
|
Dietary Management:
Recommended Foods:
- High-fiber fruits (apples, pears, berries)
- Vegetables (broccoli, peas, spinach)
- Whole grains (oatmeal, brown rice, whole wheat bread)
- Legumes (beans, lentils)
- Prune or pear juice (natural laxatives)
Foods to Limit:
- Excessive dairy products (cheese, ice cream)
- Processed foods high in fat
- White rice, white bread, pasta
- Bananas (in large quantities)
- Fast food and fried foods
Dietary Tips:
- Aim for age + 5 grams of fiber daily (e.g., 10 grams for a 5-year-old)
- Increase fiber gradually to prevent gas and bloating
- Ensure adequate fluid intake (approximately 1.5-2 liters daily for school-age children)
- Maintain a food diary to identify problematic foods
Toilet Sitting Program:
Recommended Toilet Sitting Schedule
Basic Protocol:
- Schedule toilet sitting 15-30 minutes after meals (utilizing gastrocolic reflex)
- Sit for 5-10 minutes (use timer)
- Ensure proper positioning (feet supported, comfortable position)
- Maintain consistency daily
- Create relaxed, non-pressured environment
Proper Positioning:
- Use foot stool if child’s feet don’t reach floor
- Slight forward lean with elbows on knees
- Relax abdominal muscles
- Avoid excessive straining
Behavioral Management Strategies:
- Create sticker charts or token systems
- Reward sitting attempts (regardless of outcome)
- Provide small rewards for successful bowel movements
- Consider graduated reward system
- Explain normal bowel function using age-appropriate terms
- Use drawings or diagrams to explain constipation and soiling
- Emphasize that soiling is not deliberate
- Normalize the condition
- Establish matter-of-fact clean-up protocol
- Teach proper wiping technique
- Involve child in age-appropriate clean-up
- Manage odor with appropriate strategies
- Develop discrete plan for school soiling episodes
- Provide extra clothes at school
- Identify safe bathroom location at school
- Collaborate with school nurse and teacher
Record Keeping for Home Management: Maintaining accurate records is essential for monitoring progress and adjusting interventions. Recommend families keep:
- Bowel movement diary (timing, consistency using Bristol Stool Scale, amount)
- Soiling episodes log
- Medication administration record
- Dietary intake log
- Toilet sitting compliance record
8. Behavioral Management Techniques
Effective behavioral management is central to the successful treatment of elimination disorders. These techniques complement medical interventions and address the behavioral and psychological factors that maintain these conditions.
8.1 ABC Framework for Behavioral Analysis
The ABC framework is a useful tool for analyzing behaviors related to elimination disorders:
A = Antecedent
(What happens before)
- Triggers for withholding
- Environmental factors
- Timing of fluid intake
- Psychosocial stressors
- Access to toileting facilities
B = Behavior
(What occurs)
- Enuresis episodes
- Encopresis incidents
- Holding/withholding patterns
- Toileting avoidance
- Hiding soiled underwear
C = Consequence
(What happens after)
- Parental responses
- Child’s emotional reactions
- Social consequences
- Reinforcement patterns
- Avoidance of discomfort
Using the ABC Framework: By systematically analyzing these components, nurses can help families identify patterns, triggers, and reinforcers that maintain elimination disorders. This analysis forms the basis for targeted behavioral management interventions.
8.2 Behavioral Management Strategies for Enuresis
Enuresis Alarms:
The most effective long-term behavioral management approach for nocturnal enuresis.
How Enuresis Alarms Work:
- Moisture sensor triggers alarm when wetting begins
- Child awakens and stops urination
- Over time, child learns to associate bladder fullness with waking
- Success rate: 65-80% with proper use
- Average time to success: 12-16 weeks
Implementation Tips:
- Parents should assist child to wake fully at alarm
- Complete bathroom visit even if bladder already emptied
- Reset alarm and return to bed
- Continue until 14 consecutive dry nights
- Consider “overlearning” (additional fluid before bed)
Bladder Training:
Techniques to increase functional bladder capacity and control.
Stream Interruption Exercises:
- Start and stop urine flow during voiding
- Perform 3-5 times per voiding session
- Practice 1-2 times daily (not every void)
- Helps strengthen pelvic floor muscles
Bladder Stretching:
- Gradually extend time between voidings
- Delay urination when urge is felt (initially for 5 minutes)
- Increase delay intervals gradually
- Maintain adequate overall hydration
Motivational Techniques:
- Use colorful chart with child’s input
- Award stars/stickers for dry nights
- Also reward compliance with protocol
- Exchange earned stars for small rewards
- Gradually increase criteria for rewards
- Child helps change wet bedding (age-appropriate)
- Takes ownership of alarm use and reset
- Maintains own voiding diary
- Participates in scheduling toilet visits
- Develop affirming statements with child
- “My body can stay dry all night”
- “I can wake up when I need to use the bathroom”
- Practice statements before bedtime
- Acknowledge and celebrate improvements
- Focus on effort rather than just outcomes
- Create milestone celebrations
- Maintain positivity during setbacks
8.3 Behavioral Management Strategies for Encopresis
Toilet Sitting Schedule:
Structured approach to establish regular bowel habits.
Implementation Protocol:
- Schedule 5-10 minute sitting periods after meals
- Use timer to define clear beginning and end
- Ensure proper positioning with footstool
- Maintain consistent schedule 7 days a week
- Use visual schedule for younger children
Important Considerations:
- Avoid pressure or criticism during sitting
- Provide distraction if needed (books, small toys)
- Never extend sitting time as punishment
- Reward compliance with sitting, not just production
Reward Systems:
Structured incentives to promote compliance and success.
Token Economy:
- Award tokens for compliance with toileting schedule
- Additional tokens for successful bowel movements in toilet
- Exchange tokens for small rewards or privileges
- Increase value for consecutive days of compliance
- Never remove tokens for accidents
Creating Effective Reward Systems:
- Involve child in selecting rewards
- Include immediate and delayed rewards
- Make rewards attainable but motivating
- Gradually increase criteria as child succeeds
- Celebrate milestone achievements
Cognitive-Behavioral Techniques:
- Age-appropriate explanation of gastrointestinal function
- Use simple diagrams to explain constipation and soiling
- Frame as a “medical problem” not a “behavior problem”
- Externalize the problem (“tricky bowels” vs. “your problem”)
- Child maintains own bowel diary (age-appropriate)
- Tracks compliance with medication and sitting schedule
- Records successful bowel movements
- Identifies patterns and triggers
- Teach recognition of body signals for need to defecate
- Practice identifying early warning signals
- Encourage immediate response to signals
- Use “listening to your body” imagery
- Teach diaphragmatic breathing during toilet sitting
- Use guided imagery for relaxation
- Practice progressive muscle relaxation
- Apply techniques during toilet sitting
8.4 Visual Aids and Educational Tools
Visual supports enhance understanding and compliance with behavioral management programs for elimination disorders. Effective visual tools include:
Toilet Training Visual Schedules
Step-by-step visual guides for toileting routines
- Sequential pictures of toileting steps
- Customizable for child’s specific routine
- Promotes independence
- Especially helpful for younger children and those with developmental delays
Bowel and Bladder Diaries
Record-keeping tools for tracking progress
- Visual calendars with symbols
- Sticker charts for successes
- Pictorial scales for stool consistency
- Engaging designs to increase child’s interest
Educational Materials
Resources to explain elimination disorders
- Simplified diagrams of urinary/digestive systems
- Children’s books about elimination
- Animation videos explaining the conditions
- Interactive educational games
Recommended Resources: Nurses should develop a resource library of visual aids and tools that can be shared with families. Age-appropriate materials enhance understanding and engagement with behavioral management programs.
9. Mnemonics for Nursing Practice
Mnemonics provide valuable memory aids for nursing assessment and intervention. The following mnemonics are specific to the behavioral management of elimination disorders:
D-R-Y-N-E-S-S
Mnemonic for Enuresis Management
D – Daily voiding schedule and diary keeping
R – Regulate fluid intake (timing and type)
Y – Yearly (at minimum) reassessment of progress
N – Nighttime waking for scheduled toileting
E – Enuresis alarm as primary behavioral intervention
S – Support and positive reinforcement (never punishment)
S – Sleeping position and bedtime routine optimization
S-O-I-L-I-N-G
Mnemonic for Encopresis Management
S – Schedule regular toilet sitting times
O – Optimize diet with fiber and fluids
I – Implement medication regimen as prescribed
L – Log bowel movements and soiling episodes
I – Initiate positive reinforcement system
N – Non-punitive approach to accidents
G – Gradually withdraw laxatives as bowel function improves
T-O-I-L-E-T
Mnemonic for Toilet Training Protocol
T – Timing (scheduled sitting after meals)
O – Observe for cues of readiness
I – Instruct on proper positioning
L – Limit sitting time (5-10 minutes max)
E – Encourage with positive reinforcement
T – Track progress consistently
P-A-R-E-N-T-S
Mnemonic for Family Education on Behavioral Management
P – Patience and persistence with treatment plan
A – Avoid punishment or shame for accidents
R – Reinforce positive behaviors consistently
E – Explain the condition age-appropriately
N – Normalize the experience (prevalence statistics)
T – Track progress objectively
S – Support the child emotionally throughout process
A-B-C-D-E
Mnemonic for Comprehensive Behavioral Management Approach
A – Assess thoroughly (physical, psychological, environmental factors)
B – Basic medical interventions (appropriate medications, treatment of underlying conditions)
C – Consistent routine implementation (toilet sitting schedule, fluid management)
D – Develop motivation system (rewards, positive reinforcement)
E – Educate child and family (age-appropriate explanations, demystification)
10. Case Studies
The following case studies illustrate comprehensive nursing assessment and behavioral management approaches for elimination disorders:
Case Study 1: Nocturnal Enuresis
Patient Profile:
- 7-year-old male
- Primary nocturnal enuresis
- Wets bed 5-6 nights per week
- No daytime symptoms
- Family history of bedwetting (father until age 9)
- Normal physical examination
- Normal urinalysis
Nursing Assessment Findings:
- Drinks large quantities of fluids in evening
- Very deep sleeper; difficult to wake
- Recent school stressors with transition to new grade
- Parents expressing frustration with changing sheets
- Child showing embarrassment and reluctance to discuss
- Refusing sleepovers due to bedwetting
- Previous unsuccessful attempts with restricting fluids alone
Nursing Interventions:
- Education about enuresis physiology for family
- Implementation of structured fluid management (70% before 5 PM)
- Double-voiding before bedtime
- Bedwetting alarm with parent assistance for waking
- Star chart with rewards for compliance and dry nights
- Waterproof mattress protector and layered bedding system
- Age-appropriate involvement in changing sheets
Outcomes:
After 14 weeks of consistent behavioral management, the child achieved 14 consecutive dry nights. Occasional relapses occurred during periods of stress, but were managed with return to fluid restrictions and intermittent alarm use. Complete resolution occurred by age 8.5 years.
Case Study 2: Retentive Encopresis
Patient Profile:
- 6-year-old female
- Soiling 3-4 times weekly for past 8 months
- Bowel movements every 4-5 days, large and painful
- History of constipation since age 3
- Previously toilet trained successfully
- Picky eater with low fiber intake
- No known medical conditions
Nursing Assessment Findings:
- Abdominal distention with palpable fecal mass in left lower quadrant
- Abdominal X-ray confirms significant fecal loading
- Withholding behaviors observed (crossing legs, squatting)
- Child denies soiling despite evidence
- Parents using punitive approaches for soiling episodes
- Child refusing to use school bathrooms
- Social withdrawal developing due to odor and teasing
Nursing Interventions:
- Education for parents and child about physiology of encopresis
- Initial bowel cleanout with PEG-based laxative
- Maintenance therapy with daily osmotic laxative
- Dietary modifications (increased fiber, adequate fluids)
- Scheduled toilet sitting after breakfast and dinner (10 minutes each)
- Footstool for proper positioning during defecation
- Reward system for toilet sitting compliance
- School management plan developed with school nurse
- Non-punitive approach to accidents emphasized
Outcomes:
Initial improvement in soiling after cleanout, with ongoing behavioral management protocol. Complete resolution of soiling achieved after 4 months of consistent implementation. Maintenance laxative therapy continued for 7 months, then gradually weaned. Relapse occurred during family vacation but quickly resolved with reinstitution of protocol.
Case Study 3: Combined Enuresis and Encopresis
Patient Profile:
- 8-year-old male
- Autism spectrum disorder
- Nocturnal and diurnal enuresis
- Encopresis with daily soiling
- Chronic constipation
- Limited dietary preferences
- Communication difficulties
Nursing Assessment Findings:
- Significant fecal impaction on examination
- Enlarged bladder on palpation
- UTI confirmed on urinalysis
- Sensory aversions to toilet sitting
- Communication limitations complicate understanding of bowel/bladder signals
- Parents exhausted and frustrated with ongoing issues
- Child shows distress with cleaning procedures
Nursing Interventions:
- Treatment of UTI with appropriate antibiotics
- Initial disimpaction with enemas in clinic setting
- Daily PEG laxative with medication schedule chart
- Visual schedule for toileting routine
- Sensory accommodations (padded toilet seat, weighted vest during sitting)
- Timed toilet sitting with visual timer (5 minutes, 4 times daily)
- Visual reward system with special interest rewards
- Social stories for toileting success
- Coordination with school for consistent implementation
- Parent support and respite resources provided
Outcomes:
Complex case requiring extended behavioral management approach. Encopresis improved first, with resolution after 6 months of consistent intervention. Enuresis required longer-term management with a combination of timed voiding, visual schedules, and eventually alarm therapy. Nighttime dryness achieved by age 10, with occasional relapses during illness or routine disruptions.
Key Insights from Case Studies:
- Individualized assessment is essential for effective behavioral management
- Combined approaches (medical and behavioral) yield best outcomes
- Consistency and persistence with interventions are crucial for success
- Family education and non-punitive approaches improve compliance and outcomes
- Adaptations for special populations (e.g., developmental disabilities) may be necessary
- School-based coordination enhances management effectiveness
11. Conclusion
Elimination disorders, particularly enuresis and encopresis, represent common challenges in pediatric healthcare that can significantly impact a child’s quality of life and family functioning. As these notes have demonstrated, effective management requires a comprehensive approach that addresses both physiological and behavioral aspects of these conditions.
Nurses play a crucial role in the assessment, management, and ongoing monitoring of elimination disorders. By implementing evidence-based behavioral management strategies, providing education and support to families, and coordinating care across settings, nurses can significantly improve outcomes for affected children.
Key Principles to Remember:
- Comprehensive assessment is the foundation of effective management
- Non-punitive, supportive approaches yield better outcomes
- Consistent implementation of intervention protocols is essential
- Combined medical and behavioral management strategies are most effective
- Family education and involvement improve treatment adherence
- Regular follow-up and monitoring support long-term success
Final Nursing Considerations:
- Customize interventions to the child’s developmental level and specific needs
- Support families through the often lengthy management process
- Coordinate care with other healthcare providers and school personnel
- Advocate for the child’s dignity and psychosocial well-being
- Stay updated on evidence-based behavioral management approaches
- Document interventions and outcomes thoroughly to guide ongoing care
By applying the knowledge and strategies outlined in these notes, nursing students can develop the competencies needed to provide effective, evidence-based care for children with elimination disorders, supporting them in achieving continence, preserving self-esteem, and promoting overall well-being.
12. References
- Better Health Channel. (n.d.). Behavioural disorders in children. [Better Health Victoria](https://www.betterhealth.vic.gov.au/health/healthyliving/behavioural-disorders-in-children)
- Mayo Clinic. (n.d.). Encopresis – Diagnosis and treatment. [Mayo Clinic](https://www.mayoclinic.org/diseases-conditions/encopresis/diagnosis-treatment/drc-20354500)
- Nursing.com. (n.d.). Nursing Care Plan for Enuresis/Bedwetting. [Nursing.com](https://nursing.com/lesson/nursing-care-plan-for-enuresis-bedwetting)
- Canadian Psychological Association. (2019). Psychology Works Fact Sheet: Enuresis and Encopresis in Children. [Canadian Psychological Association](https://cpa.ca/docs/File/Publications/FactSheets/PsychologyWorksFactSheet_EnuresisEncopresisInChildren_Feb2019.pdf)
- Cincinnati Children’s Hospital. (n.d.). Encopresis in Children. [Cincinnati Children’s](https://www.cincinnatichildrens.org/health/e/encopresis)
- Royal Children’s Hospital Melbourne. (n.d.). Acute behavioural disturbance: Acute management. [RCH Clinical Guide](https://www.rch.org.au/clinicalguide/guideline_index/Acute_behavioural_disturbance__Acute_management/)
- National Center for Biotechnology Information. (n.d.). Encopresis. [NCBI Bookshelf](https://www.ncbi.nlm.nih.gov/books/NBK560560/)
- NurseTogether. (n.d.). Impaired Urinary Elimination Nursing Diagnosis & Care Plans. [NurseTogether](https://www.nursetogether.com/impaired-urinary-elimination-nursing-diagnosis-care-plan/)
- Autism Little Learners. (n.d.). FREE Toileting Sequence For Autism. [Autism Little Learners](https://autismlittlelearners.com/free-toileting-sequence/)
- Beck Institute. (n.d.). Using the Mnemonic “Three Cs” with Children and Adolescents. [Beck Institute](https://beckinstitute.org/blog/using-the-mnemonic-three-cs-with-children-and-adolescents/)
- NCBI. (n.d.). Chapter 12 Childhood and Adolescence Disorders – Nursing. [National Center for Biotechnology Information](https://www.ncbi.nlm.nih.gov/books/NBK590039/)
- Nationwide Children’s Hospital. (n.d.). Enuresis (Bedwetting). [Nationwide Children’s](https://www.nationwidechildrens.org/conditions/enuresis-bedwetting)
