Upper Respiratory Tract Infections
Comprehensive Nursing Education Guide
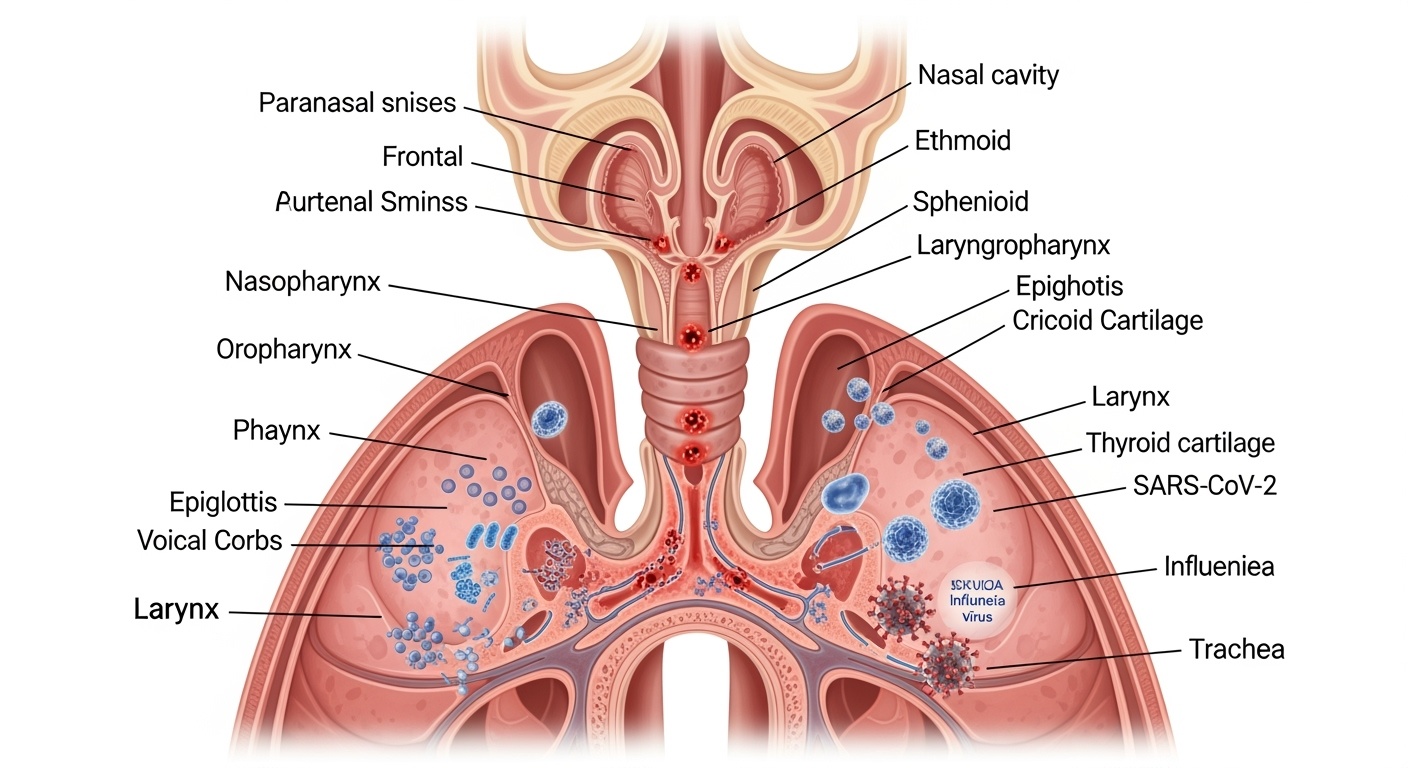
Figure 1: Upper Respiratory Tract Anatomy and Common Infection Sites
Definition & Overview
Definition
Upper Respiratory Tract Infections (URTIs) are acute infections involving the nasal cavity, paranasal sinuses, pharynx, larynx, and upper portion of the trachea. These infections predominantly affect the mucous membranes and associated lymphoid tissues above the level of the vocal cords.
Key Characteristics
- Self-limiting in most cases
- Highly contagious
- Seasonal variation common
- Affects all age groups
- Primary cause of healthcare visits
Epidemiology
- Adults: 2-4 episodes/year
- Children: 6-8 episodes/year
- Peak incidence: Fall and winter
- Leading cause of work absenteeism
Types of Upper Respiratory Tract Infections
Common Cold (Rhinitis)
Most frequent URTI affecting nasal passages and nasopharynx.
Duration: 7-10 days
Primary symptoms: Nasal congestion, rhinorrhea, sneezing
Sinusitis
Inflammation of paranasal sinuses, often following viral rhinitis.
Types: Acute, chronic, recurrent
Primary symptoms: Facial pain, pressure, thick discharge
Pharyngitis
Inflammation of pharynx and surrounding lymphoid tissue.
Types: Viral, bacterial (strep throat)
Primary symptoms: Sore throat, dysphagia, fever
Laryngitis
Inflammation of larynx and vocal cords.
Duration: 3-7 days (acute)
Primary symptoms: Hoarseness, voice loss, dry cough
Tracheitis
Inflammation of trachea, often secondary to other URTIs.
Risk: Progression to lower respiratory tract
Primary symptoms: Cough, chest discomfort, fever
Epiglottitis
Life-threatening inflammation of epiglottis (rare since Hib vaccine).
Emergency: Requires immediate intervention
Primary symptoms: Drooling, muffled voice, stridor
Memory Aid – URTI Types
Cold (Rhinitis) – Sinusitis – Pharyngitis – Laryngitis – Tracheitis – Epiglottitis
Etiological Factors
Viral Pathogens (85-95%)
Rhinoviruses
Most common cause of common cold (30-50% of cases)
Peak: Fall and spring seasons
Coronaviruses
Second most common cause (10-15% of colds)
Peak: Winter and early spring
Influenza A & B
Cause epidemic respiratory illness
Seasonal patterns, severe systemic symptoms
Parainfluenza viruses
Common in children, cause croup
Respiratory Syncytial Virus (RSV)
Significant in infants and elderly
Adenoviruses
Cause pharyngoconjunctival fever
Bacterial Pathogens (5-15%)
Streptococcus pyogenes (Group A Strep)
Leading cause of bacterial pharyngitis
Haemophilus influenzae
Sinusitis, epiglottitis (rare post-vaccine)
Streptococcus pneumoniae
Sinusitis, secondary bacterial infections
Moraxella catarrhalis
Sinusitis, particularly in COPD patients
Other Pathogens
Mycoplasma pneumoniae
Atypical pathogen, prolonged illness
Chlamydophila pneumoniae
Pharyngitis, sinusitis
Risk Factors
- Close contact exposure
- Cold, dry weather conditions
- Compromised immune system
- Very young or elderly age
- Smoking and secondhand smoke
- Crowded living conditions
- Stress and fatigue
Transmission Routes
Respiratory Droplets
Coughing, sneezing, talking (primary route)
Direct Contact
Hand-to-hand, touching contaminated surfaces
Airborne
Small particle aerosols (less common)
Pathophysiology
Infection Process Overview
Upper respiratory tract infections result from pathogen invasion of the respiratory mucosa, triggering inflammatory responses that produce the characteristic clinical manifestations. The process involves multiple interconnected mechanisms affecting respiratory epithelium, immune responses, and physiological functions.
Pathophysiological Cascade
Pathogen Entry
Viral/bacterial invasion through respiratory droplets or direct contact
Epithelial Attachment
Pathogens bind to respiratory epithelium via specific receptors
Cellular Invasion
Pathogen penetration and replication within host cells
Immune Response
Activation of innate and adaptive immune systems
Inflammatory Response
Release of inflammatory mediators and cytokines
Clinical Symptoms
Manifestation of respiratory and systemic symptoms
Cellular Level Changes
Epithelial Damage
Loss of ciliary function, disrupted barrier integrity
Mucus Hypersecretion
Goblet cell hyperplasia, increased mucin production
Vascular Changes
Vasodilation, increased permeability, edema formation
Immune Response
Innate Immunity
Neutrophil recruitment, interferon production
Adaptive Immunity
T-cell activation, antibody production
Inflammatory Mediators
Histamine, leukotrienes, prostaglandins, cytokines
Symptom Development
Nasal Symptoms
Congestion from vascular dilation, rhinorrhea from hypersecretion
Throat Symptoms
Pain from inflammation, dysphagia from edema
Systemic Symptoms
Fever from cytokine release, malaise from immune activation
Complications
- Secondary bacterial infections
- Progression to lower respiratory tract
- Chronic inflammation and tissue damage
- Exacerbation of underlying conditions
Signs & Symptoms
Objective Signs
Vital Signs
- Low-grade fever (99-101°F)
- Mild tachycardia
- Normal respiratory rate (mild increase possible)
Physical Examination
- Nasal mucosal erythema and edema
- Mucopurulent nasal discharge
- Pharyngeal erythema
- Tonsillar enlargement
- Cervical lymphadenopathy
Subjective Symptoms
Primary Complaints
- Nasal congestion
- Rhinorrhea (clear to purulent)
- Sore throat
- Dry or productive cough
- Sneezing
Associated Symptoms
- Headache (frontal, sinus pressure)
- Malaise and fatigue
- Decreased appetite
- Sleep disturbance
Typical Symptom Timeline
Onset Phase
- Scratchy throat
- Mild nasal congestion
- Sneezing
- Clear rhinorrhea
Peak Phase
- Worsening congestion
- Thicker discharge
- Sore throat pain
- Cough development
Maintenance Phase
- Persistent cough
- Thick nasal discharge
- Fatigue
- Possible fever
Resolution Phase
- Gradual improvement
- Decreasing congestion
- Residual cough
- Return of energy
Red Flag Symptoms – Immediate Medical Attention Required
Respiratory Emergency
- Stridor or severe respiratory distress
- Drooling with inability to swallow
- Muffled or “hot potato” voice
- Tripod positioning
Systemic Complications
- High fever >103°F (39.4°C)
- Severe headache with neck stiffness
- Signs of dehydration
- Altered mental status
Nursing Assessment
Comprehensive Assessment Approach
Nursing assessment of upper respiratory tract infections requires systematic evaluation of respiratory status, symptom severity, functional impact, and risk factors for complications. The assessment guides individualized nursing interventions and identifies patients requiring immediate medical attention.
Health History
Present Illness
- Onset, duration, and progression of symptoms
- Fever pattern and associated symptoms
- Characteristics of nasal discharge
- Cough type and productivity
- Self-treatment measures attempted
Past Medical History
- Previous respiratory infections frequency
- Known allergies and sensitivities
- Immunization status
- Chronic conditions (asthma, COPD, diabetes)
Physical Assessment
Vital Signs Assessment
- Temperature monitoring
- Heart rate and rhythm
- Respiratory rate and pattern
- Blood pressure
- Oxygen saturation
Head & Neck Examination
- Nasal patency and discharge character
- Sinus tenderness and swelling
- Throat erythema and exudate
- Lymph node assessment
Assessment Tools and Severity Scales
Symptom Severity Scale (0-10)
Functional Impact Assessment
- Sleep quality and duration
- Work/school attendance ability
- Appetite and nutrition status
- Activity tolerance level
- Social interaction impact
Assessment Mnemonic – “RESPIRATORY”
R – Rate (respiratory rate and pattern)
E – Effort (breathing effort, accessory muscle use)
S – Sounds (breath sounds, voice changes)
P – Position (preferred positioning, comfort)
I – Inspection (visual examination of airways)
R – Range of motion (head/neck movement)
A – Associated symptoms (fever, malaise)
T – Temperature (core body temperature)
O – Oxygenation (SpO2, skin color)
R – Risk factors (age, immunocompromised)
Y – Your patient’s concerns (patient priorities)
Diagnosis
Medical Diagnosis
Clinical Diagnosis
Primarily based on clinical presentation and physical examination. Laboratory testing generally not required for uncomplicated URTIs.
- History and symptom pattern analysis
- Physical examination findings
- Seasonal and epidemiological factors
Differential Diagnosis
- Viral vs bacterial etiology
- Allergic rhinitis
- Lower respiratory tract involvement
- Non-infectious causes
Nursing Diagnoses
Ineffective Airway Clearance
Related to increased mucus production and nasal congestion
Impaired Verbal Communication
Related to laryngeal inflammation and voice changes
Acute Pain
Related to inflammatory process in throat and sinuses
Disturbed Sleep Pattern
Related to nasal congestion and cough
Risk for Infection
Risk for secondary bacterial infection
Diagnostic Tests (When Indicated)
Rapid Strep Test
For suspected bacterial pharyngitis (GAS)
Throat Culture
If rapid strep negative but high suspicion
Nasal Culture
Chronic or recurrent sinusitis
Imaging (CT/MRI)
Complicated sinusitis or suspected complications
Red Flag Indicators
Bacterial Infection Suspicion
- • High fever >101.3°F (38.5°C)
- • Purulent nasal discharge
- • Unilateral facial pain
- • Symptoms >10 days
Serious Complications
- • Respiratory distress
- • Severe headache with neck stiffness
- • Visual changes
- • Altered mental status
Medical Management
Treatment Philosophy
Medical management of URTIs is primarily supportive, focusing on symptom relief and prevention of complications. Most URTIs are viral and self-limiting, requiring conservative treatment. Antibiotic therapy is reserved for confirmed bacterial infections or patients at high risk for complications.
Conservative Management
Rest and Hydration
- Adequate rest (7-9 hours sleep)
- Increased fluid intake (8-10 glasses/day)
- Warm liquids (tea, broth, warm water)
- Humidified environment
Natural Remedies
- Saltwater gargles (½ tsp salt in warm water)
- Honey for cough (>1 year old)
- Steam inhalation
- Saline nasal irrigation
Pharmacological Treatment
Symptom Relief Medications
Topical Treatments
- Saline nasal sprays
- Throat lozenges
- Nasal decongestant sprays (≤3 days)
Antibiotic Use Guidelines
Indications for Antibiotics
- Confirmed Group A Streptococcal pharyngitis
- Acute bacterial sinusitis (specific criteria)
- Acute otitis media with complications
- Epiglottitis (emergency treatment)
- Immunocompromised patients (selected cases)
First-Line Antibiotic Choices
- Amoxicillin: Strep throat, sinusitis
- Azithromycin: Penicillin allergy
- Clindamycin: Severe penicillin allergy
- Amoxicillin-clavulanate: Recurrent/chronic sinusitis
Treatment Decision Algorithm
• Gradual onset
• Low-grade fever
• Clear discharge
• Systemic symptoms mild
• Mixed presentation
• Moderate symptoms
• Risk factors present
Consider testing if indicated
• Sudden onset
• High fever
• Purulent discharge
• Severe symptoms
After appropriate testing
Nursing Management
Holistic Nursing Approach
Nursing management of URTIs encompasses comprehensive patient assessment, evidence-based interventions, patient education, and evaluation of outcomes. Nurses play a crucial role in promoting comfort, preventing complications, and supporting patient self-management while monitoring for signs of deterioration requiring medical intervention.
Priority Nursing Interventions
Airway Management
- Position patient to promote drainage (semi-Fowler’s position)
- Encourage fluid intake to thin secretions
- Administer humidified air/oxygen as prescribed
- Teach effective coughing techniques
- Perform nasal suctioning if needed (infants/elderly)
Comfort Measures
- Monitor temperature and provide antipyretic measures
- Offer cool/warm foods based on throat comfort
- Facilitate warm compresses for sinus pain
- Encourage voice rest for laryngitis
Infection Control & Prevention
Personal Protection
- Use appropriate PPE during patient care
- Perform frequent hand hygiene
- Maintain standard precautions
- Avoid touching face/eyes during care
Patient Isolation
- Encourage home isolation when appropriate
- Limit visitors during acute phase
- Ensure adequate room ventilation
Patient & Family Education
Self-Care Management
- Adequate hydration importance
- Rest and activity modification
- Proper medication administration
- Temperature monitoring techniques
- Humidification methods
Prevention Strategies
- Hand hygiene techniques
- Respiratory etiquette
- Vaccination importance
- Smoke avoidance
- Social distancing during illness
When to Seek Help
- High fever >103°F (39.4°C)
- Difficulty breathing
- Symptoms lasting >10 days
- Worsening symptoms
- Signs of complications
Ongoing Monitoring & Evaluation
Assessment Parameters
- Temperature trends
- Respiratory status
- Hydration status
- Sleep quality
- Nutritional intake
- Medication adherence
Outcome Indicators
- Improved symptom scores
- Return to baseline function
- Absence of complications
- Patient satisfaction
- Effective self-management
- Prevention of recurrence
Implementation in Nursing Practice
Clinical Implementation Strategy
Implementation of URTI management in nursing practice requires systematic application of evidence-based interventions across various healthcare settings. Nurses must adapt their approach based on patient populations, available resources, and institutional protocols while maintaining high standards of care and patient safety.
Acute Care Settings
Emergency Department
- Rapid triage and risk stratification
- Immediate isolation precautions
- Focused assessment for complications
- Symptomatic relief interventions
- Discharge planning and education
Inpatient Units
- Infection control protocols
- Continuous monitoring for deterioration
- Multidisciplinary collaboration
- Documentation and progress tracking
Ambulatory Care Settings
Primary Care Clinics
- Preventive care and health maintenance
- Telephone triage protocols
- Patient education programs
- Follow-up care coordination
Occupational Health
- Return-to-work assessments
- Workplace outbreak management
- Prevention program implementation
Special Population Considerations
Pediatric Patients
- Age-specific vital sign norms
- Weight-based medication dosing
- Family-centered care approach
- Immunization status verification
- Dehydration risk monitoring
Elderly Patients
- Polypharmacy considerations
- Comorbidity impact assessment
- Fall risk evaluation
- Cognitive function monitoring
- Support system assessment
Immunocompromised
- Enhanced surveillance protocols
- Strict isolation precautions
- Early physician notification
- Diagnostic test prioritization
- Lower threshold for hospitalization
Quality Improvement Initiatives
Performance Metrics
- Time to symptom relief
- Patient satisfaction scores
- Readmission/return visit rates
- Appropriate antibiotic use
- Patient education effectiveness
Improvement Strategies
- Evidence-based protocol development
- Staff education programs
- Regular outcome analysis
- Patient feedback integration
- Continuous process refinement
Implementation Mnemonic – “IMPLEMENT CARE”
I – Identify patient needs and risk factors
M – Monitor vital signs and symptoms
P – Provide comfort measures
L – Listen to patient concerns
E – Educate patient and family
M – Manage medications safely
E – Ensure infection control
N – Navigate healthcare resources
T – Track progress and outcomes
C – Coordinate multidisciplinary care
A – Advocate for patient needs
R – Reassess and modify care plan
E – Evaluate intervention effectiveness
