Protein Energy Malnutrition (PEM)
Comprehensive Nursing Notes for Clinical Practice
Learning Objectives
Knowledge Goals:
- Define protein energy malnutrition and its global impact
- Identify causes and risk factors for PEM
- Classify different types of malnutrition
- Recognize clinical manifestations of PEM
Clinical Skills:
- Assess nutritional status using standardized tools
- Implement evidence-based nursing interventions
- Develop prevention strategies for at-risk populations
- Collaborate in multidisciplinary care teams
Visual Classification of Protein Energy Malnutrition
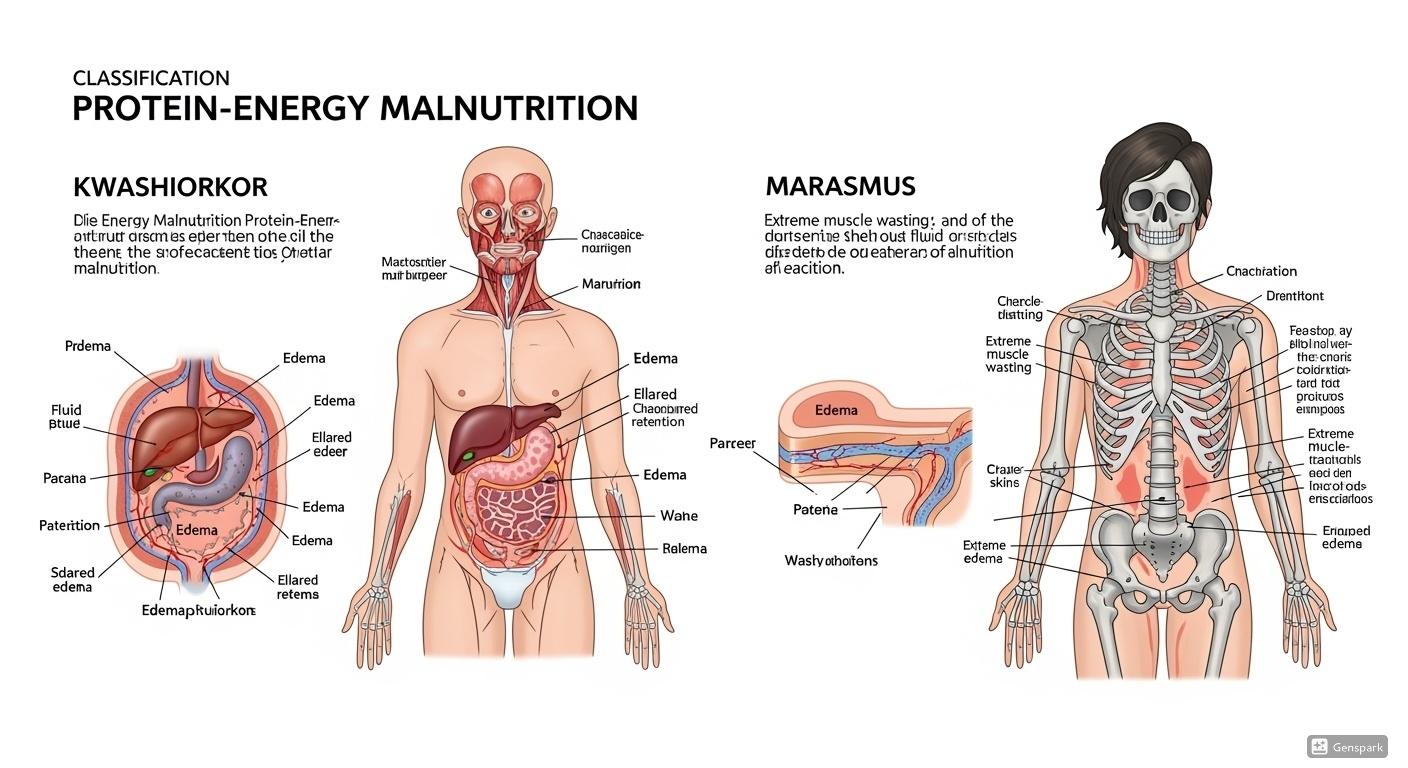
Comparative visualization of malnutrition types showing key diagnostic features
1. Magnitude of the Problem
Global Impact
Protein Energy Malnutrition affects approximately 1 in 4 children worldwide, with the highest prevalence in Sub-Saharan Africa and South Asia. It remains the leading cause of childhood mortality, contributing to 45% of all deaths in children under 5 years of age.
Epidemiological Trends
- Stunting: Decreased from 32.5% (2000) to 22.0% (2020)
- Wasting: Remains stable at 6.7% globally
- Underweight: Declined from 25.0% (2000) to 13.6% (2020)
- Severe Acute Malnutrition: Affects 13.6 million children annually
2. Causes and Risk Factors
Multifactorial Etiology of PEM
Immediate Causes
- Insufficient protein and energy intake
- Poor food quality and diversity
- Inappropriate feeding practices
- Diarrheal diseases
- Respiratory infections
- Parasitic infections
- HIV/AIDS
Underlying Causes
- Limited access to nutritious foods
- Economic constraints
- Seasonal food shortages
- Poor breastfeeding practices
- Inadequate maternal knowledge
- Limited healthcare access
Mnemonic: FEEDS
- Food insecurity and poverty
- Education and knowledge deficits
- Environmental factors (sanitation, water)
- Diseases and infections
- Social and cultural factors
Clinical Pearl: Remember that malnutrition is rarely due to a single cause but results from the complex interaction of multiple factors. Address all contributing factors for effective intervention.
High-Risk Populations
- Children 6-24 months
- Pregnant women
- Lactating mothers
- Elderly individuals
- Chronic diseases
- Immunocompromised states
- Gastrointestinal disorders
- Metabolic disorders
- Extreme poverty
- Displacement/refugees
- Single-parent households
- Limited education
3. Classification of Malnutrition
Primary Classification Systems
| Classification | Type | Key Features | Clinical Presentation |
|---|---|---|---|
| Marasmus | Severe wasting |
|
|
| Kwashiorkor | Protein deficiency |
|
|
| Marasmic-Kwashiorkor | Mixed type |
|
|
WHO Growth Standards
MUAC Classification
Memory Aid: MAK Classification
- Monkey face appearance
- Muscle atrophy
- No edema
- Edema present
- Hair changes
- Skin lesions
- Mixed presentation
- Most severe form
- Highest mortality
4. Signs and Symptoms
Clinical Manifestations by System
Growth and Development
- • Stunted growth (height-for-age deficit)
- • Delayed motor development
- • Delayed cognitive development
- • Delayed puberty
- • Reduced muscle mass
Dermatological Changes
- • Dry, scaly skin
- • Hyperpigmentation
- • Skin ulcers and wounds
- • Delayed wound healing
- • Desquamation
Hair Changes
- • Hair depigmentation
- • Fine, sparse hair
- • Easy hair plucking
- • Flag sign (alternating bands)
- • Brittle hair texture
Cardiovascular System
- • Bradycardia
- • Hypotension
- • Reduced cardiac output
- • Arrhythmias
- • Peripheral edema
Respiratory System
- • Respiratory muscle weakness
- • Reduced lung capacity
- • Increased infection risk
- • Impaired cough reflex
- • Dyspnea on exertion
Neurological System
- • Apathy and irritability
- • Reduced mental alertness
- • Delayed reflexes
- • Cognitive impairment
- • Behavioral changes
Clinical Pearl: Early Warning Signs
- Loss of interest in play
- Increased irritability
- Social withdrawal
- Reduced appetite
- Failure to gain weight
- Frequent infections
- Delayed wound healing
- Fatigue and weakness
Mnemonic: MALNOURISHED
- Muscle wasting
- Apathy and irritability
- Loss of subcutaneous fat
- No interest in surroundings
- Oedema (in kwashiorkor)
- Under-weight for age
- Reduced immunity
- Infections (frequent)
- Skin changes
- Hair changes
- Energy deficiency
- Delayed growth
5. Severe Acute Malnutrition (SAM)
Emergency Recognition Criteria
- Weight-for-height <-3 SD (Z-score)
- MUAC <11.5 cm (children 6-59 months)
- Bilateral nutritional edema
- Inability to feed
- Persistent vomiting
- Lethargy/unconsciousness
- Convulsions
SAM Management Protocol
SAM Management Flowchart
Outpatient Care (OTP)
Inpatient Care (SC)
Outpatient Treatment (OTP)
- Ready-to-Use Therapeutic Food (RUTF)
- Weekly follow-up visits
- Amoxicillin for 7 days
- Measles vaccination
- Deworming
Inpatient Treatment (SC)
- Stabilization phase (F-75)
- Rehabilitation phase (F-100)
- Follow-up phase (RUTF)
Clinical Pearl: The 10 Steps of SAM Management
- Treat/prevent hypoglycemia
- Treat/prevent hypothermia
- Treat/prevent dehydration
- Correct electrolyte imbalance
- Treat infections
- Cautious feeding
- Catch-up growth
- Provide micronutrients
- Provide loving care
- Prepare for discharge
6. Management and Prevention
Therapeutic Management
Nutritional Rehabilitation
- • Gradual increase in caloric intake
- • High-energy, high-protein foods
- • Frequent small meals (6-8 times daily)
- • Micronutrient supplementation
- • Monitor for refeeding syndrome
Medical Management
- • Antibiotic therapy (amoxicillin)
- • Vitamin A supplementation
- • Folic acid and iron supplements
- • Zinc supplementation
- • Treatment of complications
Monitoring Parameters
- • Daily weight measurements
- • Fluid intake and output
- • Vital signs monitoring
- • Electrolyte balance
- • Signs of infection
Psychosocial Support
- • Emotional support for family
- • Play therapy for children
- • Family counseling
- • Support groups
- • Discharge planning
Prevention Strategies
Primary Prevention
- • Exclusive breastfeeding (0-6 months)
- • Appropriate complementary feeding
- • Food security programs
- • Maternal education
- • Water and sanitation
Secondary Prevention
- • Growth monitoring
- • Early detection programs
- • Community screening
- • Vaccination programs
- • Deworming programs
Tertiary Prevention
- • Rehabilitation programs
- • Follow-up care
- • Relapse prevention
- • Long-term monitoring
- • Community integration
Mnemonic: PREVENT
- Protein-energy adequate diet
- Regular growth monitoring
- Education of caregivers
- Vaccination programs
- Early detection and treatment
- Nutrition counseling
- Treatment of infections
7. Nurses’ Role in PEM Management
Core Nursing Responsibilities
Assessment and Screening
- • Anthropometric measurements
- • Nutritional assessment
- • Clinical examination
- • Risk factor identification
- • Family and social assessment
Care Planning
- • Develop individualized care plans
- • Set realistic goals
- • Coordinate multidisciplinary care
- • Plan discharge and follow-up
- • Document care outcomes
Direct Care Provision
- • Feeding assistance
- • Medication administration
- • Wound care
- • Infection prevention
- • Comfort measures
Education and Counseling
- • Nutrition education
- • Breastfeeding support
- • Hygiene practices
- • Medication compliance
- • Follow-up care instructions
Community Outreach
- • Health screening programs
- • Community education
- • Support group facilitation
- • Referral services
- • Advocacy for resources
Monitoring and Evaluation
- • Progress monitoring
- • Complication surveillance
- • Outcome evaluation
- • Quality improvement
- • Data collection and reporting
Nursing Process Application
Nursing Process in PEM Care
- • Anthropometry
- • Clinical signs
- • Dietary history
- • Social factors
- • Imbalanced nutrition
- • Risk for infection
- • Deficient knowledge
- • Altered growth
- • Set goals
- • Prioritize needs
- • Plan interventions
- • Resource allocation
- • Nutritional support
- • Education
- • Monitoring
- • Coordination
- • Weight gain
- • Improved appetite
- • Reduced infections
- • Family knowledge
Clinical Pearl: Nursing Priorities in PEM
- Stabilize vital signs
- Prevent complications
- Initiate feeding protocol
- Monitor for refeeding syndrome
- Provide comfort measures
- Achieve catch-up growth
- Prevent recurrence
- Educate family
- Ensure follow-up care
- Promote health maintenance
Professional Development
Continuing Education
- • Attend nutrition workshops
- • Join professional organizations
- • Pursue specialized certifications
- • Participate in research
- • Stay updated with guidelines
Interprofessional Collaboration
- • Work with dietitians
- • Coordinate with physicians
- • Collaborate with social workers
- • Engage community health workers
- • Partner with NGOs
Summary and Key Takeaways
Essential Points to Remember
- • PEM affects 1 in 4 children globally, contributing to 45% of under-5 deaths
- • Early recognition and intervention are crucial for optimal outcomes
- • Management requires a comprehensive, multidisciplinary approach
- • Prevention strategies are more cost-effective than treatment
- • Nurses play pivotal roles in all aspects of PEM care
- • Community-based interventions are essential for sustainable impact
Clinical Practice Guidelines
- • Use standardized assessment tools (WHO growth charts, MUAC)
- • Follow evidence-based treatment protocols
- • Monitor for complications and adverse reactions
- • Provide family-centered care
- • Ensure continuity of care through proper discharge planning
- • Advocate for policy changes and resource allocation
Final Mnemonic: NURSING EXCELLENCE
- Nutritional assessment and intervention
- Understanding of pathophysiology
- Recognition of warning signs
- Support for families
- Infection prevention
- Networking with multidisciplinary teams
- Growth monitoring
- Education and counseling
- Xpert clinical skills
- Community outreach
- Evaluation of outcomes
- Long-term follow-up
- Leadership in prevention
- Empowerment of caregivers
- Never-ending learning
- Continuous quality improvement
- Ethical practice
Commitment to Excellence in Nursing Care
These comprehensive notes serve as a foundation for evidence-based nursing practice in protein energy malnutrition management. Continue to stay updated with the latest research and guidelines to provide the best possible care for vulnerable populations.
