Asepsis, Infection Control & Wound Healing
Comprehensive Nursing Education Notes
Table of Contents
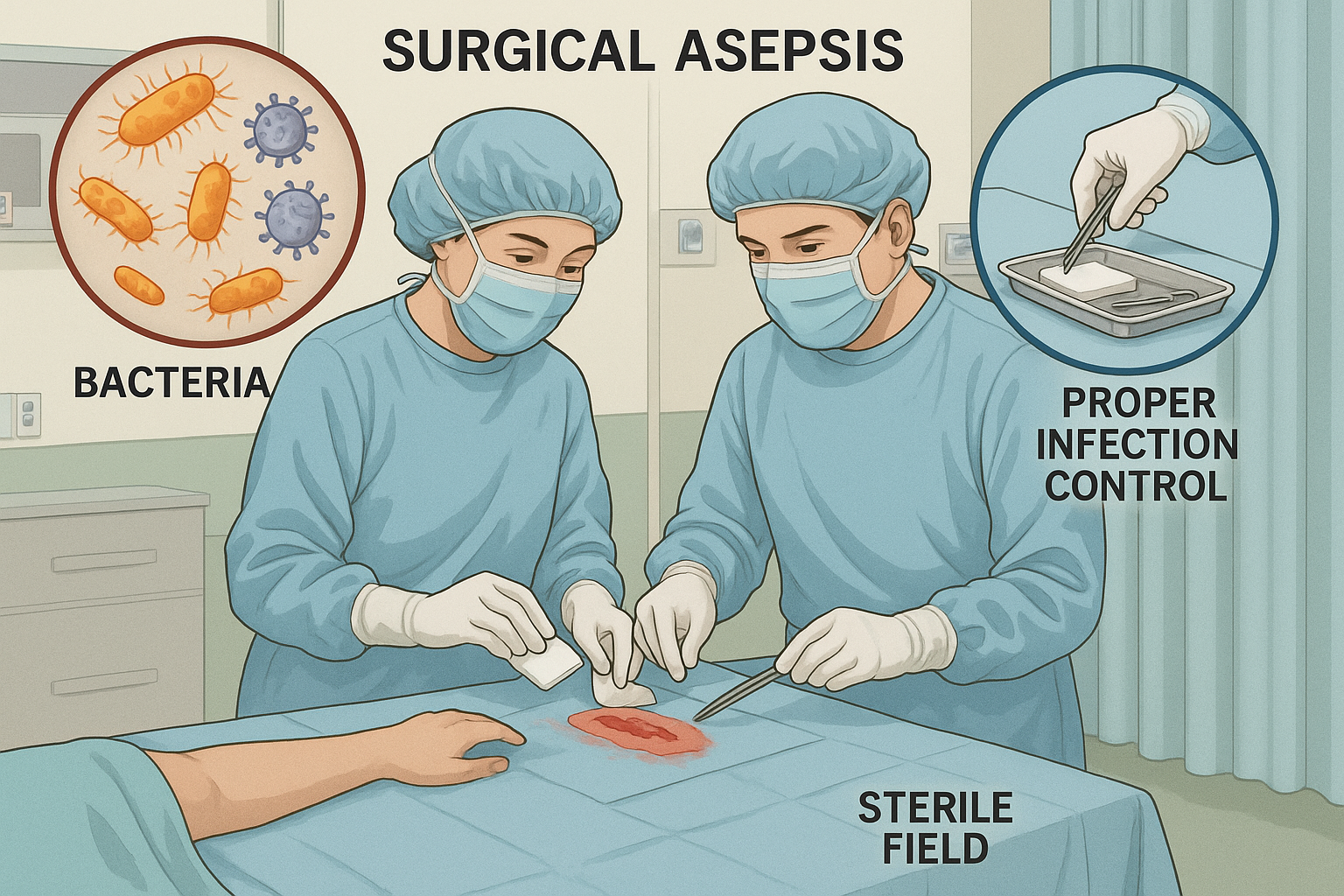
Professional aseptic technique in clinical practice
1. Introduction to Medical and Surgical Asepsis
Core Concept
Asepsis refers to the absence of pathogenic microorganisms, forming the foundation of infection prevention and control in healthcare settings. It encompasses practices, procedures, and techniques designed to prevent the transmission of microorganisms between patients, healthcare workers, and the environment.
1.1 Medical vs Surgical Asepsis
Medical Asepsis (Clean Technique)
- Reduces number of pathogenic organisms
- Prevents spread of microorganisms
- Used in routine patient care
- Includes hand hygiene, PPE, environmental cleaning
Surgical Asepsis (Sterile Technique)
- Complete absence of microorganisms
- Maintains sterile field
- Used during invasive procedures
- Requires sterile supplies and environment
Memory Aid: STERILE Technique Principles
S – Sterile items touch only sterile items
T – Time limits apply to sterile fields
E – Edges of sterile fields are not sterile
R – Reach around, not over sterile fields
I – Items below waist level are contaminated
L – Liquids flow toward contamination
E – Exposure to air contaminates sterile items
1.2 Core Principles of Asepsis
Chain of Infection Prevention
Breaking any link in this chain prevents infection transmission
2. Inflammation and Infection
2.1 The Inflammatory Process
Inflammation is the body’s protective response to tissue injury, irritation, or infection. It serves to eliminate harmful stimuli, remove damaged cells, and initiate tissue repair processes.
Cardinal Signs of Inflammation: PRISH
P – Pain (Dolor)
R – Redness (Rubor)
I – Increased temperature (Calor)
S – Swelling (Tumor)
H – Loss of function (Functio laesa)
Phases of Inflammatory Response
Phase 1: Vascular Response (0-30 minutes)
- • Immediate vasoconstriction (5-10 seconds)
- • Followed by vasodilation
- • Increased vascular permeability
- • Plasma exudation and edema formation
Phase 2: Cellular Response (30 minutes – hours)
- • Neutrophil migration and activation
- • Phagocytosis of pathogens and debris
- • Release of inflammatory mediators
- • Complement cascade activation
Phase 3: Resolution and Repair (hours – days)
- • Macrophage infiltration
- • Debris clearance
- • Anti-inflammatory mediator release
- • Tissue regeneration initiation
2.2 Types of Infections
Healthcare-Associated Infections (HAIs)
- CAUTI: Catheter-associated UTI
- CLABSI: Central line-associated bloodstream infection
- SSI: Surgical site infections
- VAP: Ventilator-associated pneumonia
- CDI: Clostridioides difficile infection
Common Pathogenic Organisms
- Gram-positive: Staphylococcus, Streptococcus
- Gram-negative: E. coli, Pseudomonas
- MDRO: MRSA, VRE, CRE
- Fungal: Candida, Aspergillus
- Viral: Influenza, COVID-19, RSV
3. Wound Healing
3.1 Stages of Wound Healing
Wound healing is a complex, dynamic process involving coordinated interactions between different cell types, extracellular matrix components, and soluble mediators. Understanding these stages is crucial for effective wound management and promoting optimal healing outcomes.
Stage 1: Hemostasis (0-24 hours)
Primary Hemostasis:
- • Immediate vasoconstriction
- • Platelet plug formation
- • von Willebrand factor activation
- • Temporary bleeding control
Secondary Hemostasis:
- • Coagulation cascade activation
- • Fibrin clot formation
- • Clot stabilization
- • Definitive hemostasis
Stage 2: Inflammatory Phase (1-6 days)
Early Inflammation (0-3 days):
- • Neutrophil infiltration
- • Bacterial clearance
- • Debris removal
- • Cytokine release
Late Inflammation (3-6 days):
- • Macrophage dominance
- • Growth factor secretion
- • Angiogenesis initiation
- • Fibroblast recruitment
Stage 3: Proliferative Phase (4-21 days)
Granulation Formation:
- • Fibroblast proliferation
- • Collagen synthesis (Type III)
- • New blood vessel formation
- • Granulation tissue development
Re-epithelialization:
- • Epithelial cell migration
- • Basement membrane restoration
- • Wound contraction
- • Myofibroblast activity
Stage 4: Maturation/Remodeling (21 days – 1+ year)
Early Remodeling (3 weeks – 6 months):
- • Collagen reorganization
- • Type III to Type I collagen conversion
- • Increased tensile strength
- • Scar tissue formation
Late Remodeling (6 months – 2 years):
- • Collagen cross-linking
- • Scar maturation
- • Maximum tensile strength (80%)
- • Final wound appearance
Memory Aid: HIPPR for Wound Healing Stages
H – Hemostasis (bleeding stops)
I – Inflammatory (cleaning begins)
P – Proliferative (building up)
R – Remodeling (strengthening)
3.2 Factors Influencing Wound Healing
Factors That Impair Healing
Local Factors:
- • Infection and biofilm formation
- • Tissue hypoxia and poor circulation
- • Foreign bodies and debris
- • Excessive wound tension
- • Inappropriate dressing selection
Systemic Factors:
- • Advanced age (>65 years)
- • Diabetes mellitus and hyperglycemia
- • Malnutrition and protein deficiency
- • Immunosuppression
- • Smoking and substance abuse
- • Chronic diseases (kidney, liver)
- • Certain medications (steroids, NSAIDs)
Factors That Promote Healing
Local Factors:
- • Adequate oxygenation and perfusion
- • Moist wound environment
- • Appropriate temperature (37°C)
- • Optimal pH levels (6.5-8.5)
- • Minimal tissue trauma
Systemic Factors:
- • Younger age and good health status
- • Optimal nutrition and hydration
- • Adequate protein intake (1.2-1.5 g/kg)
- • Sufficient vitamin C, A, and zinc
- • Good glycemic control
- • Non-smoking status
- • Adequate sleep and stress management
4. Wound Care and Dressing Techniques
4.1 Comprehensive Wound Assessment
Thorough wound assessment is the foundation of effective wound management. It involves systematic evaluation of multiple parameters to determine appropriate treatment strategies and monitor healing progress.
Memory Aid: WOUND ASSESSMENT Using “TIMERS”
T – Tissue type and viability
I – Infection signs
M – Moisture level
E – Edges and epithelialization
R – Radiation (size and depth)
S – Surrounding skin condition
Wound Dimensions
- Length: Head to toe measurement
- Width: Side to side measurement
- Depth: Surface to deepest point
- Undermining: Tissue loss beneath intact skin
- Tunneling: Narrow passageway extending from wound
Tissue Types
- Granulation: Red, bumpy, healthy healing tissue
- Epithelial: Pink/purple tissue at wound edges
- Slough: Yellow/tan devitalized tissue
- Eschar: Black/brown necrotic tissue
- Hypergranulation: Excessive granulation tissue
Drainage Assessment
- Serous: Clear, thin, watery
- Serosanguineous: Pink/light red, thin
- Sanguineous: Red, contains RBCs
- Purulent: Thick, opaque, infected
- Amount: Scant, minimal, moderate, copious
4.2 Dressing Selection and Techniques
Dressing Selection Algorithm
Hydrogels, Hydrocolloids
Foams, Composites
Alginates, Superabsorbents
Modern Wound Dressing Categories
Primary Dressings (Contact Wound Bed):
- Hydrogels: 90% water, maintains moisture, cools wound
- Hydrocolloids: Absorb exudate, form gel, autolytic debridement
- Alginates: High absorption, hemostatic properties, biodegradable
- Foams: Absorb exudate, thermal insulation, cushioning
- Antimicrobials: Silver, honey, iodine-based infection control
Secondary Dressings (Over Primary):
- Transparent Films: Waterproof, allow gas exchange, visual monitoring
- Gauze: Traditional, versatile, requires frequent changes
- Composite: Multiple layers, combine absorption with protection
- Compression: Edema reduction, venous return improvement
- Tapes/Adhesives: Secure dressings, minimize skin trauma
Sterile Dressing Change Procedure
Preparation Phase:
- Verify physician orders and patient identity
- Gather supplies and equipment
- Explain procedure to patient
- Position patient for optimal access
- Perform hand hygiene and don PPE
- Prepare sterile field and supplies
Implementation Phase:
- Remove old dressing using clean technique
- Assess wound and document findings
- Cleanse wound with appropriate solution
- Apply new dressing using sterile technique
- Secure dressing appropriately
- Dispose of materials safely
- Document procedure and findings
Memory Aid: WOUND CARE Principles “MOIST”
M – Maintain moist environment
O – Optimize nutrition and oxygenation
I – Infection prevention and control
S – Support patient comfort and mobility
T – Temperature maintenance (body temperature)
5. Nursing Implementation and Clinical Applications
Evidence-Based Practice Integration
Effective nursing implementation of asepsis and wound care principles requires integration of current evidence-based practices, critical thinking skills, and patient-centered care approaches. Nurses serve as the primary coordinators of wound management and infection prevention strategies across all healthcare settings.
Core Nursing Responsibilities
Assessment and Monitoring:
- • Comprehensive wound assessment using validated tools
- • Infection surveillance and early recognition
- • Pain assessment and management strategies
- • Nutritional screening and intervention needs
- • Patient mobility and functional status evaluation
- • Psychosocial impact assessment
Intervention and Care Coordination:
- • Implementation of evidence-based wound care protocols
- • Aseptic technique maintenance during all procedures
- • Patient and family education programs
- • Interdisciplinary team collaboration
- • Quality improvement initiatives
- • Discharge planning and continuity of care
Clinical Decision-Making Framework
Nursing Process Application in Wound Care
ASSESS
Comprehensive wound evaluation
DIAGNOSE
Identify nursing problems
PLAN
Set measurable outcomes
IMPLEMENT
Execute interventions
EVALUATE
Monitor progress
Specialized Clinical Applications
Acute Care Settings
Surgical Wound Management:
- • Post-operative incision monitoring
- • Surgical site infection prevention
- • Drain and tube site care
- • Early mobilization protocols
Critical Care Considerations:
- • Pressure injury prevention in immobile patients
- • Medical device-related pressure injuries
- • Moisture-associated skin damage prevention
- • Infection control in immunocompromised patients
Community and Home Care
Patient Education Priorities:
- • Proper hand hygiene techniques
- • Signs and symptoms of infection
- • Dressing change procedures
- • When to seek medical attention
Family/Caregiver Training:
- • Aseptic technique principles
- • Wound assessment documentation
- • Nutritional support strategies
- • Emergency response protocols
Long-term Care Facilities
Preventive Strategies:
- • Comprehensive skin assessment protocols
- • Pressure redistribution systems
- • Incontinence-associated dermatitis prevention
- • Nutrition and hydration optimization
Chronic Wound Management:
- • Diabetic ulcer prevention and care
- • Venous insufficiency management
- • Pressure injury staging and treatment
- • Pain management strategies
Clinical Excellence Framework: “CARING WOUNDS”
C – Comprehensive assessment
A – Aseptic technique maintenance
R – Risk factor identification
I – Infection prevention protocols
N – Nutritional optimization
G – Goal-oriented care planning
W – Wound-appropriate dressing selection
O – Ongoing monitoring and evaluation
U – Understanding patient perspectives
N – Nursing documentation excellence
D – Discharge planning coordination
S – Safety and quality assurance
Quality Indicators and Outcome Measures
Process Indicators
- Hand hygiene compliance
- Dressing change frequency
- Documentation completeness
Outcome Indicators
- Wound healing rates
- Infection rates
- Patient satisfaction scores
Structure Indicators
- Staff competency levels
- Resource availability
- Policy adherence rates
Professional Development and Continuing Education
Core Competencies for Nurses:
- • Advanced wound assessment skills
- • Infection prevention and control knowledge
- • Critical thinking and clinical reasoning
- • Evidence-based practice integration
- • Patient education and counseling abilities
- • Interdisciplinary collaboration skills
Certification Opportunities:
- • Wound, Ostomy and Continence Nursing (WOCN)
- • Certified Wound Care Nurse (CWS)
- • Infection Control and Prevention (CIC)
- • Medical-Surgical Nursing (CMSRN)
- • Critical Care Nursing (CCRN)
- • Gerontological Nursing (RN-BC)
