Lung Cysts and Tumors
Comprehensive Nursing Notes
Evidence-Based Clinical Guide for Nursing Students
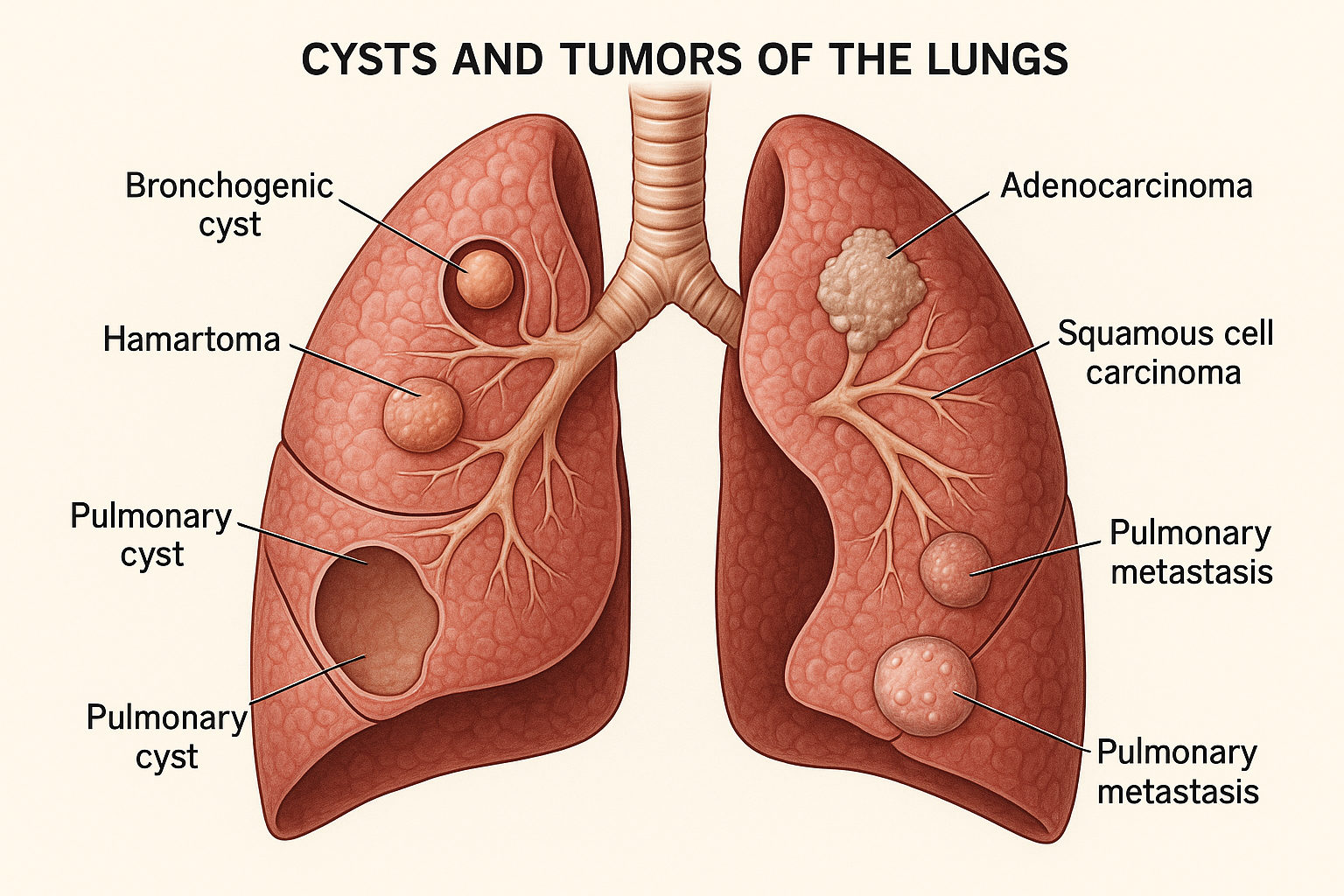
Figure 1: Anatomical representation of various lung cysts and tumors
Definition and Overview
Lung Cysts
Lung cysts are abnormal, air-filled spaces within the lung parenchyma that are bounded by an epithelial or fibrous wall. These structures are typically larger than 1 cm in diameter and appear as round, well-defined, thin-walled lesions on imaging studies. Cysts can be congenital (present from birth) or acquired throughout life due to various pathological processes.
Key Characteristics:
- • Thin-walled (≤2mm)
- • Well-circumscribed
- • Contains air or fluid
- • Size >1cm diameter
Lung Tumors
Lung tumors represent abnormal proliferation of cells within the pulmonary tissue, which can be benign (non-cancerous) or malignant (cancerous). These masses result from uncontrolled cellular growth and can originate from various lung structures including bronchi, alveoli, pleura, or blood vessels. Lung tumors are a leading cause of cancer-related mortality worldwide.
Classification:
- • Primary vs. Metastatic
- • Benign vs. Malignant
- • Central vs. Peripheral
- • Cell type specific
Memory Aid: CYST vs TUMOR
CYST:
C – Circumscribed (well-defined)
Y – Yielding air/fluid content
S – Single wall structure
T – Thin-walled appearance
TUMOR:
T – Tissue proliferation
U – Uncontrolled growth
M – Mass effect present
O – Organ dysfunction potential
R – Risk of malignancy
Types of Lung Cysts and Tumors
Lung Cysts
Congenital Cysts
- Bronchogenic Cysts: Most common, arise from abnormal budding of the tracheobronchial tree
- Congenital Pulmonary Airway Malformation (CPAM): Multicystic mass replacing normal lung tissue
- Pulmonary Sequestration: Non-functioning lung tissue with aberrant blood supply
- Congenital Lobar Emphysema: Progressive overdistention of alveolar spaces
Acquired Cysts
- Pneumatoceles: Thin-walled air cysts following pneumonia
- Blebs and Bullae: Air-filled spaces from alveolar wall destruction
- Parasitic Cysts: Echinococcal (hydatid) cysts from parasite infection
- Post-infectious Cysts: Result from necrotizing infections
Systemic Disease Cysts
- Lymphangioleiomyomatosis (LAM): Progressive cystic destruction in women
- Langerhans Cell Histiocytosis: Multisystem disorder with pulmonary cysts
- Birt-Hogg-Dubé Syndrome: Genetic disorder with multiple pulmonary cysts
Lung Tumors
Primary Malignant Tumors
- Non-Small Cell Lung Cancer (NSCLC) – 85%:
- – Adenocarcinoma (40%): Most common, often peripheral
- – Squamous Cell Carcinoma (25%): Often central, cavitation common
- – Large Cell Carcinoma (10%): Poorly differentiated, aggressive
- Small Cell Lung Cancer (SCLC) – 15%: Highly aggressive, central location
- Rare Primary Tumors: Carcinoid, sarcomas, lymphomas
Metastatic Tumors
- Common Primary Sites:
- – Breast (most common in women)
- – Colon and rectum
- – Kidney (renal cell carcinoma)
- – Prostate, melanoma, sarcomas
- Patterns: Multiple nodules, cannonball lesions
Benign Tumors
- Hamartomas: Most common benign tumor, contains cartilage and fat
- Adenomas: Rare benign epithelial tumors
- Arteriovenous Malformations: Vascular malformations
- Inflammatory Pseudotumors: Non-neoplastic inflammatory masses
Clinical Pearl: The “Rule of Thirds”
For solitary pulmonary nodules: 1/3 are malignant, 1/3 are benign neoplasms, and 1/3 are inflammatory/infectious. Size matters: nodules >3cm have 80% malignancy risk, while those <1cm have <5% risk.
Etiological Factors
Cyst Formation Factors
Developmental Factors
- • Abnormal embryonic development
- • Genetic mutations (FLCN, TSC1, TSC2)
- • Chromosomal abnormalities
- • Failure of normal branching morphogenesis
Acquired Factors
- • Infections (bacterial, viral, parasitic)
- • Inflammatory conditions
- • Trauma and barotrauma
- • Autoimmune diseases
- • Drug-induced lung injury
Environmental Factors
- • Smoking and air pollution
- • Occupational exposures
- • Mechanical ventilation
- • High altitude exposure
Tumor Development Factors
Primary Risk Factors
- • Smoking: 85% of lung cancers, 20-fold increased risk
- • Radon exposure: Second leading cause
- • Occupational carcinogens: Asbestos, chromium, nickel
- • Air pollution: PM2.5, diesel exhaust
Genetic Factors
- • Family history of lung cancer
- • p53, KRAS, EGFR mutations
- • Li-Fraumeni syndrome
- • Hereditary retinoblastoma
Secondary Factors
- • Previous lung disease (COPD, pulmonary fibrosis)
- • Prior radiation therapy
- • Immunosuppression
- • Age (peak incidence 55-65 years)
- • Gender (historically male predominant)
Mnemonic: SMOKE-R for Lung Cancer Risk Factors
S – Smoking (primary)
M – Metastasis (secondary)
O – Occupational exposure
K – Kinship (family history)
E – Environmental toxins
R – Radon exposure
Pathophysiology
Cyst Pathophysiology
Cyst Formation Process
Initial insult (developmental, inflammatory, infectious)
Tissue destruction or abnormal development
Cavity formation with epithelial lining
Air trapping and cyst expansion
Physiological Effects
- Ventilation: V/Q mismatch, dead space ventilation
- Compression: Adjacent lung tissue compression
- Infection risk: Poor drainage, bacterial colonization
- Pneumothorax: Rupture risk, especially with thin-walled cysts
Tumor Pathophysiology
Carcinogenesis Process
DNA damage from carcinogens
Oncogene activation, tumor suppressor loss
Abnormal cellular proliferation
Invasion and metastasis potential
Tumor Effects
- Mass effect: Airway obstruction, lung collapse
- Vascular invasion: Hemoptysis, pulmonary embolism
- Paraneoplastic: SIADH, hypercalcemia, neuropathy
- Metastatic spread: Lymphatic, hematogenous routes
Cellular and Molecular Mechanisms
Cyst Formation
- • Matrix metalloproteinase activation
- • Inflammatory mediator release
- • Epithelial-mesenchymal transition
- • Abnormal elastin/collagen balance
Tumor Growth
- • Growth factor overexpression
- • Angiogenesis stimulation
- • Apoptosis resistance
- • Cell cycle checkpoint loss
Signs and Symptoms
Mnemonic: CHEST-PAIN for Respiratory Symptoms
C – Cough (persistent)
H – Hemoptysis
E – Exercise intolerance
S – Shortness of breath
T – Thoracic pain
P – Pneumothorax risk
A – Abnormal breath sounds
I – Infection recurrent
N – Night sweats
Lung Cysts
Asymptomatic Presentation (Common)
- • Incidental finding on imaging (50-70%)
- • Routine chest X-ray discovery
- • No functional impairment
- • Normal exercise tolerance
Symptomatic Presentation
- Respiratory:
- – Dyspnea on exertion
- – Chronic cough (dry or productive)
- – Recurrent respiratory infections
- Chest Pain:
- – Pleuritic chest pain
- – Sudden onset if pneumothorax
Complications
- • Pneumothorax: Sudden chest pain, dyspnea
- • Infection: Fever, purulent sputum, malaise
- • Hemoptysis: Blood-tinged sputum
- • Compression: Atelectasis, mediastinal shift
Lung Tumors
Early Symptoms (Often Subtle)
- • Persistent cough (>3 weeks)
- • Change in chronic cough pattern
- • Mild dyspnea on exertion
- • Fatigue and decreased appetite
- • Chest discomfort or aching
Advanced Symptoms
- Pulmonary:
- – Hemoptysis (blood-streaked sputum)
- – Severe dyspnea, orthopnea
- – Chest pain (constant, severe)
- – Recurrent pneumonia
- Systemic:
- – Unintentional weight loss >5%
- – Night sweats, fever
- – Bone pain (metastasis)
Paraneoplastic Syndromes
- • SIADH: Hyponatremia, confusion
- • Hypercalcemia: Fatigue, constipation, kidney stones
- • Cushing’s syndrome: Central obesity, moon facies
- • Lambert-Eaton syndrome: Muscle weakness
- • Hypertrophic pulmonary osteoarthropathy: Joint pain, clubbing
Red Flag Symptoms Requiring Immediate Attention
Emergency
- • Massive hemoptysis
- • Severe dyspnea at rest
- • Chest pain + dyspnea
Urgent
- • New hemoptysis
- • Superior vena cava syndrome
- • Vocal cord paralysis
Priority
- • Unexplained weight loss
- • Persistent cough >3 weeks
- • New dyspnea
Nursing Assessment
Assessment Mnemonic: RESPIRATORY
R – Respiratory rate, rhythm, effort
E – Exercise tolerance assessment
S – Sputum characteristics
P – Pain assessment (location, quality)
I – Inspection (chest wall, clubbing)
R – Risk factors identification
A – Auscultation findings
T – Tactile fremitus, percussion
O – Oxygen saturation monitoring
R – Review of systems
Y – Yearly screening compliance
Primary Assessment
Health History
- Chief Complaint: Onset, duration, severity (0-10 scale)
- Smoking History: Pack-years calculation
- Occupational: Asbestos, chemicals, dust exposure
- Family History: Lung cancer, genetic disorders
- Previous Imaging: Comparison studies availability
- Medications: Current and recent drug history
Physical Examination
- Vital Signs:
- – Temperature (fever suggests infection)
- – Respiratory rate (normal: 12-20/min)
- – Blood pressure, heart rate
- – Oxygen saturation (room air and exercise)
- General Appearance:
- – Cachexia, weight loss
- – Use of accessory muscles
- – Positioning preferences
Inspection
- Chest Wall:
- – Symmetry, deformities
- – Breathing pattern (regular, labored)
- – Chest expansion equality
- Extremities:
- – Digital clubbing (>160° nail angle)
- – Cyanosis (central vs. peripheral)
- – Edema, lymphadenopathy
Advanced Assessment
Palpation
- Tactile Fremitus:
- – Increased: consolidation, mass
- – Decreased: pleural effusion, pneumothorax
- – Absent: complete obstruction
- Chest Expansion: Measure with tape measure
- Lymph Nodes: Supraclavicular, axillary palpation
Percussion
- Normal: Resonant sound
- Dullness: Mass, consolidation, pleural effusion
- Hyperresonance: Pneumothorax, large cyst
- Diaphragmatic excursion: Measure movement
Auscultation
- Breath Sounds:
- – Decreased/absent: mass, effusion
- – Bronchial: consolidation
- – Wheeze: airway obstruction
- Adventitious Sounds:
- – Crackles: infection, edema
- – Pleural friction rub: pleural inflammation
- – Stridor: upper airway obstruction
Functional Assessment
- Exercise Tolerance:
- – Stairs climbed without SOB
- – Distance walked before dyspnea
- – Activities of daily living impact
- Quality of Life: Sleep, appetite, mood
Assessment Documentation Framework
Objective Data
- • Vital signs trends
- • Physical findings
- • Functional measurements
- • Laboratory values
Subjective Data
- • Symptom descriptions
- • Pain scales (0-10)
- • Patient concerns
- • Functional limitations
Risk Stratification
- • High-risk features
- • Complication potential
- • Monitoring needs
- • Priority interventions
Diagnostic Procedures
Imaging Studies
Chest X-ray (Initial screening)
- Cysts: Round, thin-walled, air-filled lesions
- Tumors: Nodules, masses, hilar enlargement
- Limitations: 25% miss rate for nodules <1cm
- Views: PA and lateral recommended
- Cost: Low, widely available
CT Chest (Gold standard)
- High-resolution CT (HRCT): Best for cysts
- Contrast-enhanced: Tumor characterization
- Sensitivity: Detects nodules >2mm
- Staging: Lymph nodes, metastases
- Follow-up: Growth rate assessment
Advanced Imaging
- PET-CT: Metabolic activity, staging
- MRI: Superior soft tissue contrast
- Ultrasound: Pleural-based lesions
- Angiography: Vascular malformations
Tissue Sampling
Non-surgical Biopsy
- CT-guided needle biopsy:
- – 90% diagnostic accuracy
- – Pneumothorax risk 20-25%
- – Outpatient procedure
- Bronchoscopy with biopsy:
- – Central lesions preferred
- – BAL for infection workup
- – EBUS for lymph nodes
Surgical Biopsy
- VATS (Video-assisted thoracoscopic surgery):
- – Minimally invasive
- – High diagnostic yield
- – Therapeutic potential
- Open thoracotomy: Complex cases
- Mediastinoscopy: Lymph node sampling
Cytological Studies
- Sputum cytology: 3 early morning samples
- Pleural fluid analysis: Effusions
- Fine needle aspiration: Lymph nodes
- Bronchial washings: Central lesions
Laboratory Tests
Baseline Labs
- • Complete blood count
- • Comprehensive metabolic panel
- • Liver function tests
- • Coagulation studies
- • Arterial blood gas
Tumor Markers
- • CEA (carcinoembryonic antigen)
- • NSE (neuron-specific enolase)
- • CYFRA 21-1
- • SCC (squamous cell carcinoma)
- • ProGRP (SCLC marker)
Molecular Testing
- • EGFR mutations
- • ALK rearrangements
- • ROS1 translocations
- • PD-L1 expression
- • KRAS mutations
Diagnostic Mnemonic: BIOPSY-CT
B – Baseline imaging (CXR)
I – Invasive sampling needed
O – Optimal technique selection
P – PET-CT for staging
S – Sputum cytology trials
Y – Yield assessment important
C – CT-guided procedures
T – Tissue confirmation essential
Diagnostic Algorithm
Step 1: Clinical assessment + Chest X-ray
Step 2: CT chest with contrast (if abnormal CXR)
Step 3: Risk stratification (size, morphology, patient factors)
Step 4: Tissue sampling (if indicated) or surveillance
Step 5: Staging workup (if malignant)
Medical Management
Lung Cysts Management
Conservative Management
- Observation: Asymptomatic cysts <4cm
- Serial imaging: CT at 3, 6, 12, 24 months
- Infection prevention: Pneumococcal, influenza vaccines
- Activity modification: Avoid high-altitude, diving
- Smoking cessation: Reduces pneumothorax risk
Medical Therapy
- Bronchodilators: If airflow limitation
- Antibiotics: Acute infections
- Anti-inflammatory: Systemic conditions (LAM)
- Sirolimus: LAM-specific therapy
- Oxygen therapy: Hypoxemic patients
Surgical Indications
- • Recurrent pneumothorax (>2 episodes)
- • Size >4cm with symptoms
- • Infection complications
- • Compression of vital structures
- • Diagnostic uncertainty
- • High-risk occupations (pilots, divers)
Surgical Options
- VATS resection: Minimally invasive preferred
- Cyst decortication: Preserve lung tissue
- Segmentectomy: Anatomical resection
- Lobectomy: Extensive disease
- Pleurodesis: Recurrent pneumothorax
Lung Tumors Management
Surgical Treatment (NSCLC)
- Lobectomy: Standard for stage I-II
- Segmentectomy: Limited pulmonary reserve
- Wedge resection: Small peripheral tumors
- Pneumonectomy: Central tumors
- VATS approach: When technically feasible
- Lymph node dissection: Staging and treatment
Chemotherapy
- Adjuvant: Stages II-III after surgery
- Neoadjuvant: Downstaging before surgery
- Palliative: Advanced disease, symptom control
- Common regimens:
- – Platinum-based doublets (cisplatin/carboplatin)
- – Taxanes, gemcitabine, pemetrexed
Targeted Therapy
- EGFR inhibitors: Erlotinib, gefitinib, osimertinib
- ALK inhibitors: Crizotinib, alectinib, ceritinib
- ROS1 inhibitors: Crizotinib, entrectinib
- BRAF inhibitors: Dabrafenib + trametinib
- Anti-angiogenic: Bevacizumab, ramucirumab
Immunotherapy
- PD-1/PD-L1 inhibitors:
- – Pembrolizumab (first-line high PD-L1)
- – Nivolumab, atezolizumab
- Combination therapy: With chemotherapy
- Duration: Continue until progression
Radiation Therapy
- SBRT: Early stage, medically inoperable
- Concurrent chemoRT: Stage III NSCLC
- Palliative RT: Bone mets, brain mets, SVC syndrome
- Prophylactic cranial irradiation: SCLC
Treatment Decision Mnemonic: STAGE-FIT
S – Stage determination
T – Tumor characteristics
A – Age and comorbidities
G – General performance status
E – Expected outcomes
F – Functional capacity
I – Individual preferences
T – Treatment goals
Supportive Care Measures
Symptom Management
- • Pain control protocols
- • Dyspnea management
- • Cough suppressants
- • Nutritional support
Complications
- • Infection prophylaxis
- • Thromboembolic prevention
- • Immunosuppression management
- • Electrolyte monitoring
Psychosocial
- • Counseling services
- • Support groups
- • Advance directives
- • Family education
Nursing Management
Nursing Care Mnemonic: BREATHE-CARE
B – Breathing pattern assessment
R – Respiratory status monitoring
E – Education and support
A – Airway clearance techniques
T – Treatment compliance
H – Hemodynamic stability
E – Emergency preparedness
C – Comfort measures
A – Activity tolerance
R – Risk factor modification
E – Emotional support
Priority Nursing Diagnoses
Primary Diagnoses
- • Impaired Gas Exchange r/t altered lung tissue
- • Ineffective Breathing Pattern r/t pain, anxiety
- • Acute Pain r/t surgical intervention, disease process
- • Risk for Infection r/t compromised lung tissue
- • Activity Intolerance r/t impaired oxygenation
Secondary Diagnoses
- • Anxiety r/t diagnosis, prognosis uncertainty
- • Ineffective Coping r/t life-threatening illness
- • Imbalanced Nutrition r/t decreased appetite, treatment effects
- • Deficient Knowledge r/t disease process, treatment
- • Risk for Pneumothorax r/t cyst rupture
Nursing Interventions by Phase
Pre-operative/Pre-treatment Phase
Assessment
- • Baseline vital signs, O2 saturation
- • Respiratory pattern, effort
- • Pain level (0-10 scale)
- • Anxiety level assessment
- • Knowledge deficit identification
Interventions
- • Pre-operative teaching
- • Smoking cessation counseling
- • Pulmonary function optimization
- • Nutritional assessment
- • Emotional support provision
Intra-operative/Acute Treatment Phase
Monitoring
- • Continuous cardiac monitoring
- • Respiratory status q15min initially
- • Chest tube output/air leak
- • Pain assessment q2-4h
- • Fluid balance monitoring
Interventions
- • Position for optimal ventilation
- • Early mobilization protocol
- • Incentive spirometry q2h
- • Multimodal pain management
- • Infection prevention measures
Post-operative/Recovery Phase
Ongoing Assessment
- • Daily weight, I&O balance
- • Wound healing assessment
- • Functional status evaluation
- • Treatment response monitoring
- • Side effect identification
Interventions
- • Progressive activity program
- • Patient education reinforcement
- • Discharge planning coordination
- • Follow-up appointment scheduling
- • Support system mobilization
Specialized Nursing Considerations
Chest Tube Management
- Assessment: Drainage amount, color, consistency
- Air leak monitoring: Continuous vs. intermittent
- Suction settings: Usually -20cmH2O
- Positioning: Keep collection system below chest level
- Patient mobility: Encourage despite tubes
- Removal criteria: <150ml/24h, no air leak
Chemotherapy Nursing
- Pre-medication: Anti-emetics, pre-hydration
- Monitoring: Vital signs, extravasation signs
- Side effect management: Nausea, fatigue, neuropathy
- Lab monitoring: CBC, comprehensive metabolic panel
- Infection precautions: Neutropenia protocol
- Patient education: Side effects, when to call
Quality Indicators for Nursing Care
Safety Metrics
- • Fall prevention
- • Medication errors
- • Infection rates
- • Pressure injury prevention
Clinical Outcomes
- • Length of stay
- • Readmission rates
- • Complication rates
- • Pain management scores
Patient Experience
- • Satisfaction scores
- • Communication ratings
- • Education effectiveness
- • Discharge readiness
Professional Practice
- • Evidence-based care
- • Care coordination
- • Documentation quality
- • Continuing education
Nursing Implementation
Patient Education Implementation
Disease Process Education
- Teaching methods: Visual aids, models, videos
- Content areas:
- – Anatomy and physiology review
- – Disease progression understanding
- – Treatment options explanation
- – Expected outcomes discussion
- Assessment: Return demonstration, verbal feedback
- Documentation: Learning objectives met/not met
Self-Care Management
- Symptom monitoring:
- – When to seek immediate care
- – Daily symptom tracking tools
- – Emergency action plans
- Medication management:
- – Proper administration techniques
- – Side effect recognition
- – Drug interaction awareness
Respiratory Care Implementation
Airway Clearance Techniques
Incentive Spirometry
- • Frequency: Every 2 hours while awake
- • Target: 10 breaths per session
- • Goal: Sustained inspiration 3-5 seconds
- • Monitor: Volume achievement
Coughing Techniques
- • Controlled coughing method
- • Splinting for post-operative patients
- • Huffing technique for weak patients
- • Positioning for effectiveness
Positioning
- • Semi-Fowler’s for comfort
- • Side-lying for drainage
- • Tripod position for dyspnea
- • Frequent position changes
Oxygen Therapy Management
Administration
- • Target SpO2: 88-92% (COPD) or >95%
- • Device selection: Nasal cannula vs. mask
- • Flow rate titration protocols
- • Humidification for high flows
- • Safety precautions (fire hazard)
Monitoring
- • Continuous pulse oximetry
- • ABG analysis as indicated
- • Respiratory rate and effort
- • Skin integrity around device
- • Patient tolerance assessment
Pain Management Implementation
Multimodal Pain Approach
Pharmacological
- • Scheduled vs. PRN dosing
- • Opioid rotation strategies
- • Adjuvant medications
- • Side effect monitoring
- • Addiction risk assessment
Non-pharmacological
- • Heat/cold therapy
- • Relaxation techniques
- • Distraction methods
- • Massage therapy
- • Positioning for comfort
Assessment
- • Regular pain scales (0-10)
- • Functional impact evaluation
- • Sleep pattern assessment
- • Breakthrough pain identification
- • Response to interventions
Psychosocial Support Implementation
Emotional Support Strategies
- Therapeutic communication:
- – Active listening techniques
- – Empathy expression
- – Open-ended questioning
- – Reflection and validation
- Coping assessment:
- – Previous coping strategies
- – Current stressors identification
- – Support system availability
Family Support Integration
- Education provision:
- – Disease process understanding
- – Care participation training
- – Emergency response plans
- Resource connection:
- – Support group referrals
- – Social work consultation
- – Spiritual care services
Implementation Mnemonic: IMPLEMENT
I – Individualized care plans
M – Monitor outcomes continuously
P – Patient education priority
L – Listen to patient concerns
E – Evidence-based interventions
M – Modify plans as needed
E – Evaluate effectiveness regularly
N – Navigate care transitions
T – Team collaboration essential
Implementation Evaluation Criteria
Short-term Goals (24-48 hours)
- • Adequate pain control (<4/10)
- • Stable vital signs
- • Effective breathing patterns
- • Absence of complications
Medium-term Goals (1 week)
- • Improved activity tolerance
- • Demonstrated self-care abilities
- • Effective coping strategies
- • Family involvement in care
Long-term Goals (Discharge)
- • Return to baseline function
- • Knowledge of follow-up care
- • Appropriate resource utilization
- • Quality of life maintenance
Complications and Prognosis
Complications
Immediate Complications
- Pneumothorax: 15-20% risk with cysts
- Hemoptysis: Risk of airway obstruction
- Respiratory failure: Acute decompensation
- Infection: Pneumonia, abscess formation
- Superior vena cava syndrome: Central tumors
Treatment-related Complications
- Post-operative:
- – Air leaks, bleeding
- – Wound infections
- – Respiratory complications
- Chemotherapy: Neuropathy, nephrotoxicity
- Radiation: Pneumonitis, fibrosis
Long-term Complications
- Functional decline: Reduced lung capacity
- Recurrence: Local or distant
- Secondary malignancies: Treatment-induced
- Chronic pain: Post-thoracotomy syndrome
- Pulmonary hypertension: Advanced disease
Prognostic Factors
Favorable Prognosis
- Cysts:
- – Asymptomatic presentation
- – Small size (<4cm)
- – Stable on imaging
- Tumors:
- – Early stage (I-II)
- – Complete resection
- – Good performance status
Survival Statistics (Lung Cancer)
- 5-year survival rates:
- – Stage I: 68-92%
- – Stage II: 53-60%
- – Stage III: 13-36%
- – Stage IV: 0-10%
- Overall: 18% five-year survival
Quality of Life Factors
- Functional status: ECOG performance scale
- Symptom burden: Dyspnea, pain levels
- Social support: Family, community resources
- Psychological well-being: Depression, anxiety
- Financial impact: Treatment costs, work ability
Complication Prevention Mnemonic: PREVENT
P – Pulmonary hygiene protocols
R – Risk factor modification
E – Early detection of changes
V – Vaccination compliance
E – Exercise and rehabilitation
N – Nutritional optimization
T – Treatment adherence
Clinical Summary
Key Clinical Points
Lung Cysts
- • Often asymptomatic, incidental findings
- • Size and symptoms guide management decisions
- • Conservative management preferred when possible
- • Pneumothorax risk requires patient education
- • Good prognosis with appropriate management
Lung Tumors
- • Early detection crucial for outcomes
- • Staging determines treatment approach
- • Multimodal therapy often required
- • Supportive care essential throughout treatment
- • Prognosis varies significantly by stage
Nursing Excellence Priorities
Assessment Excellence
- • Comprehensive respiratory assessment
- • Early recognition of complications
- • Functional status monitoring
- • Psychosocial needs identification
Intervention Excellence
- • Evidence-based care protocols
- • Patient-centered education
- • Collaborative care coordination
- • Comfort and quality of life focus
Outcome Excellence
- • Complication prevention
- • Optimal functional outcomes
- • Patient satisfaction achievement
- • Care transition success
Future Considerations
Emerging Treatments
- • Precision medicine approaches
- • Novel targeted therapies
- • Immunotherapy combinations
- • Minimally invasive techniques
- • CAR-T cell therapies
Nursing Practice Evolution
- • Advanced practice roles expansion
- • Technology integration in care
- • Population health focus
- • Preventive care emphasis
- • Survivorship care models
Study Success Tips for Nursing Students
Review Regularly
Revisit key concepts weekly to reinforce learning
Practice Application
Use case studies and clinical scenarios
Use Mnemonics
Leverage memory aids provided in this guide
Clinical Connection
Connect theory to patient care experiences
