Surgical Safety
Complete Guide for Nursing Students
Master perioperative protocols and patient safety measures
Introduction to Surgical Safety
Surgical safety represents the cornerstone of modern perioperative nursing practice, encompassing comprehensive protocols designed to prevent adverse events and ensure optimal patient outcomes. As healthcare professionals, nurses play a pivotal role in maintaining the highest standards of surgical safety throughout the entire perioperative continuum.
Key Learning Objectives
- Understand the fundamental principles of surgical safety protocols
- Master preoperative, intraoperative, and postoperative safety measures
- Identify and prevent common surgical complications
- Apply evidence-based practices in perioperative care
- Implement effective communication strategies in surgical settings
Statistics Impact
Proper surgical safety protocols reduce adverse events by up to 47% and decrease mortality rates by 23% according to WHO Safe Surgery initiatives.
Team Approach
Effective surgical safety requires coordinated efforts from surgeons, anesthesiologists, nurses, and support staff working as a cohesive team.
Preoperative Safety Protocols
The preoperative phase is critical for establishing the foundation of surgical safety. During this phase, nurses must conduct thorough assessments, verify patient information, and ensure all safety protocols are implemented before the patient enters the operating room.
Patient Identification and Verification
| Verification Step | Method | Documentation |
|---|---|---|
| Patient Identity | Two identifiers (name, DOB, MRN) | Wristband verification |
| Surgical Procedure | Consent form review | Surgical schedule confirmation |
| Surgical Site | Site marking with patient awake | Marking verification checklist |
| Allergies | Patient interview and chart review | Allergy band placement |
Preoperative Mnemonic: “SAFETY FIRST”
S – Site marking verified
A – Allergies documented
F – Fasting status confirmed
E – Equipment functioning
T – Team communication
Y – Yes, consent obtained
F – Fluids and medications
I – Identity confirmed
R – Records complete
S – Surgical timeout
T – Transfer preparation
Physical Assessment
- Vital signs baseline
- Cardiovascular status
- Respiratory function
- Neurological assessment
- Skin integrity
Documentation Review
- Medical history
- Medication list
- Laboratory results
- Imaging studies
- Consent forms
Patient Education
- Procedure explanation
- Postoperative expectations
- Pain management
- Recovery timeline
- Discharge planning
Intraoperative Safety Measures
During the surgical procedure, maintaining surgical safety requires constant vigilance and adherence to sterile technique, continuous patient monitoring, and effective team communication. The intraoperative phase presents unique challenges that demand immediate response and expert nursing judgment.
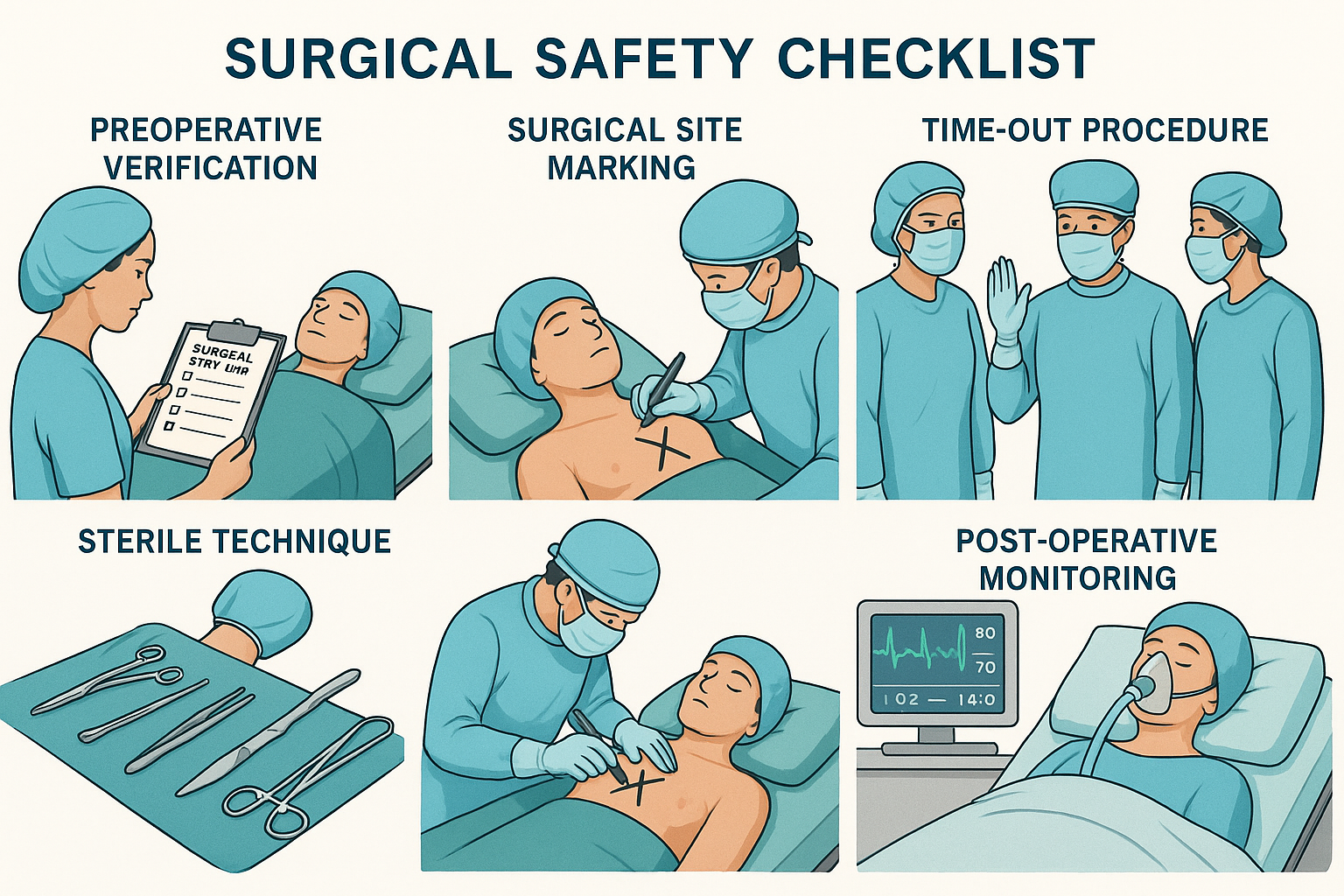
WHO Surgical Safety Checklist Implementation
Sign In (Before Induction)
- Patient identity confirmed
- Site and procedure verified
- Consent obtained and documented
- Site marked and visible
- Safety checks completed
- Known allergies discussed
- Pulse oximeter functioning
Time Out (Before Incision)
- Team member introductions
- Patient, site, procedure confirmation
- Anticipated critical events review
- Antibiotic prophylaxis timing
- Essential imaging displayed
- Equipment concerns addressed
- Sterility confirmation
Sign Out (Before Leaving OR)
- Procedure name confirmed
- Needle, sponge, instrument counts
- Specimen labeling verified
- Equipment problems identified
- Key concerns for recovery
- Postoperative orders reviewed
- Team debrief completed
Sterile Technique Maintenance
Four Fundamental Principles
1. Know what is sterile
Only items processed through sterilization are considered sterile until contaminated.
2. Know what is not sterile
Anything not processed or compromised becomes contaminated immediately.
3. Separate sterile from non-sterile
Maintain clear boundaries between sterile and non-sterile areas.
4. Remedy contamination immediately
Address any breach in sterility without delay or compromise.
Intraoperative Monitoring Parameters
Postoperative Monitoring and Safety
Postoperative surgical safety focuses on continuous patient assessment, early detection of complications, and implementation of appropriate interventions. This phase requires heightened awareness of potential adverse events and systematic monitoring protocols.
Post-Anesthesia Care Unit (PACU) Assessment
PACU Mnemonic: “RECOVERY”
R – Respiratory status
E – Elimination patterns
C – Circulation assessment
O – Oxygenation monitoring
V – Vital signs stability
E – Emotional support
R – Range of motion
Y – Yes to pain management
| Assessment Area | Normal Findings | Red Flags | Interventions |
|---|---|---|---|
| Airway | Clear, patent, no stridor | Obstruction, snoring, stridor | Position, suction, airway device |
| Breathing | Regular, unlabored, SpO2 >95% | Irregular, labored, SpO2 <90% | Oxygen therapy, positioning |
| Circulation | Stable BP, regular pulse | Hypotension, tachycardia | Fluid replacement, medications |
| Consciousness | Appropriate response to stimuli | Delayed emergence, confusion | Stimulation, reversal agents |
Postoperative Pain Management
Pain Assessment Tools
- Numeric Rating Scale (0-10): Most common for alert patients
- Wong-Baker FACES: Pediatric and cognitively impaired
- PQRST Method: Comprehensive pain evaluation
- Behavioral Indicators: Non-verbal patients
- Physiological Signs: Vital sign changes
Multimodal Approach
- Pharmacological: Opioids, NSAIDs, adjuvants
- Regional Anesthesia: Nerve blocks, epidural
- Non-pharmacological: Ice, positioning, distraction
- Patient-controlled: PCA pumps for appropriate patients
- Preventive: Pre-emptive analgesia strategies
Preventing Surgical Complications
Prevention of surgical complications is fundamental to surgical safety practice. Understanding risk factors, implementing evidence-based interventions, and maintaining vigilant monitoring are essential components of comprehensive perioperative care.
Surgical Complications Incidence
Surgical Site Infections (SSI)
Prevention Strategies:
- Appropriate antibiotic prophylaxis timing
- Optimal glucose control (≤180 mg/dL)
- Maintenance of normothermia
- Hair removal with clippers, not razors
- Chlorhexidine-alcohol skin preparation
Target: SSI rate <2% for clean procedures
Venous Thromboembolism (VTE)
Prevention Measures:
- Risk assessment using validated tools
- Mechanical prophylaxis (compression devices)
- Pharmacological prophylaxis when indicated
- Early mobilization protocols
- Adequate hydration maintenance
Goal: VTE rate reduction by 50%
Pressure Injuries
Prevention Protocol:
- Risk assessment (Braden Scale)
- Appropriate positioning and padding
- Regular position changes
- Skin integrity monitoring
- Pressure-redistributing surfaces
Target: Zero preventable pressure injuries
Respiratory Complications
Prevention Strategies:
- Preoperative pulmonary function optimization
- Smoking cessation counseling
- Incentive spirometry education
- Early mobilization and ambulation
- Proper pain management for effective coughing
Goal: Pneumonia rate <1% for elective surgery
Risk Assessment and Stratification
| Risk Factor | Assessment Tool | High Risk Indicators | Interventions |
|---|---|---|---|
| VTE Risk | Caprini Score | Score ≥3 | Anticoagulation, compression |
| Pressure Injury | Braden Scale | Score ≤18 | Positioning, padding, monitoring |
| Cardiac Risk | RCRI Score | ≥2 risk factors | Cardiac evaluation, optimization |
| SSI Risk | NNIS Risk Index | Score 2-3 | Enhanced prophylaxis protocol |
Global Best Practices in Surgical Safety
Leading healthcare systems worldwide have implemented innovative surgical safety practices that demonstrate measurable improvements in patient outcomes. These evidence-based approaches serve as models for enhancing surgical safety protocols globally.
Mayo Clinic (USA)
Team-Based Safety Culture
- STAR Program: Structured teamwork and communication
- Safety Huddles: Daily multidisciplinary briefings
- Peer Review Process: Continuous improvement through feedback
- Simulation Training: Regular team-based scenario practice
Results: 40% reduction in preventable harm events
NHS England (UK)
Never Events Prevention
- LocSSIP: Local Safety Standards for Invasive Procedures
- NatSSIPs: National Safety Standards implementation
- Surgical Safety Thermometer: Real-time safety monitoring
- Learning System: Incident analysis and sharing
Results: 50% reduction in never events over 5 years
Singapore Health (Singapore)
Technology-Enhanced Safety
- RFID Tracking: Real-time instrument and sponge counting
- AI-Powered Monitoring: Predictive analytics for complications
- Digital Checklists: Automated compliance monitoring
- Telemedicine Integration: Remote specialist consultation
Results: 99.9% accuracy in surgical counts
Karolinska (Sweden)
Patient-Centered Safety
- Patient Engagement: Active involvement in safety checks
- Family Integration: Family members as safety partners
- Cultural Competency: Culturally sensitive care protocols
- Shared Decision Making: Collaborative treatment planning
Results: 95% patient satisfaction with safety communication
Implementation Framework for Best Practices
Assess
Current state analysis and gap identification
Plan
Strategy development and resource allocation
Implement
Phased rollout with training and support
Monitor
Performance measurement and continuous improvement
Key Performance Indicators for Surgical Safety
| Category | Metric | Target | Measurement Frequency |
|---|---|---|---|
| Process | WHO Checklist Compliance | 100% | Daily |
| Outcome | Surgical Site Infection Rate | <2% | Monthly |
| Safety | Never Events | 0 | Continuous |
| Experience | Patient Safety Satisfaction | >90% | Quarterly |
Key Takeaways for Nursing Students
Essential Principles
- • Surgical safety is a multidisciplinary responsibility
- • Prevention is more effective than treatment
- • Communication failures are leading causes of errors
- • Continuous monitoring prevents complications
- • Evidence-based protocols save lives
Nursing Excellence
- • Master systematic assessment techniques
- • Develop strong communication skills
- • Embrace lifelong learning and improvement
- • Practice with compassion and competence
- • Lead by example in safety culture
“Excellence in surgical safety is not an accident. It is the result of high intention, sincere effort, and skilled execution.”
