Prevention of IV Complications
Comprehensive Nursing Study Guide
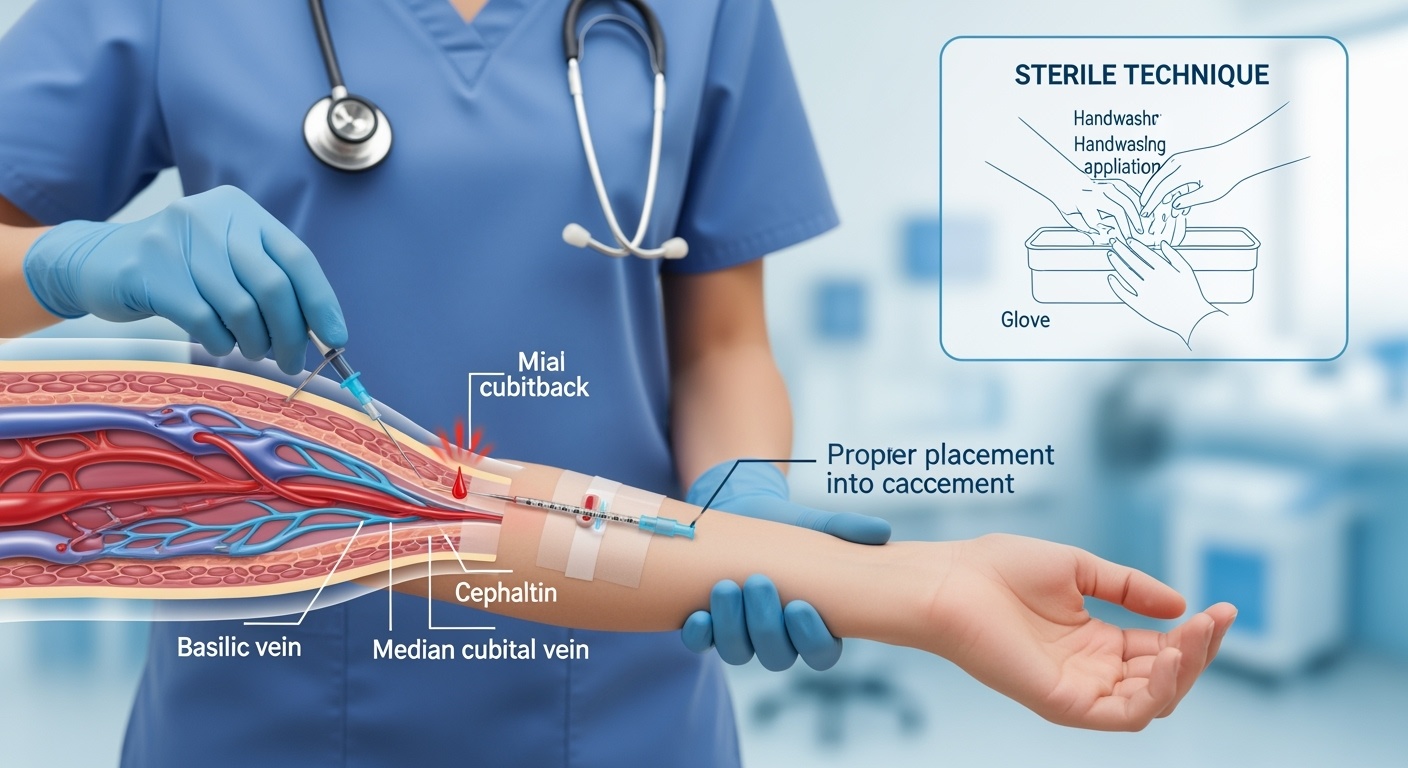
Professional IV insertion demonstrating proper sterile technique and anatomical considerations
Table of Contents
- 1. Introduction to IV Complications
- 2. Common IV Complications
- 3. Risk Factors Assessment
- 4. Prevention Strategies
- 5. Sterile Technique Protocols
- 6. Monitoring and Assessment
- 7. Nursing Implementation
- 8. Key Memory Aids
1. Introduction to IV Complications
Intravenous (IV) therapy is one of the most common medical procedures performed in healthcare settings, with over 80% of hospitalized patients receiving IV treatment. Despite its routine nature, IV therapy carries significant risks for complications that can range from minor local reactions to life-threatening systemic infections. Understanding prevention strategies is crucial for nursing practice and patient safety.
Statistical Overview
- • 15-25% of patients develop IV-related complications
- • Phlebitis occurs in 20-80% of IV insertions
- • Infiltration affects 11-58% of IV sites
- • PICC-related infections: 2.4 per 1000 catheter days
Learning Objectives
- • Identify major IV complications and risk factors
- • Apply evidence-based prevention strategies
- • Demonstrate proper assessment techniques
- • Implement quality improvement measures
2. Common IV Complications
Phlebitis
Definition: Inflammation of the vein wall
Types:
- • Mechanical: Catheter size/movement
- • Chemical: Medication irritation
- • Bacterial: Infection-related
Signs: Redness, warmth, swelling, pain, palpable cord
Infiltration/Extravasation
Definition: Fluid leakage into surrounding tissue
Differences:
- • Infiltration: Non-vesicant fluids
- • Extravasation: Vesicant/caustic drugs
Signs: Swelling, coolness, pain, blanching, slowed infusion
Catheter-Related Bloodstream Infection (CRBSI)
Definition: Systemic infection originating from IV catheter
Risk Factors: Central lines, immunocompromised patients, prolonged catheterization
Signs: Fever, chills, positive blood cultures, exit site drainage
Occlusion/Thrombosis
Definition: Blockage of catheter lumen or vessel
Types: Fibrin sheath, blood clot, precipitate formation
Signs: Inability to flush, aspirate, or infuse; alarm activation
3. Risk Factors Assessment
Risk Assessment Framework
Patient Factors
Device Factors
Procedural Factors
Environmental
Patient Factors
- • Age (pediatric/elderly)
- • Immunocompromised status
- • Diabetes mellitus
- • Poor vascular access
- • Previous IV complications
- • Skin integrity issues
Device Factors
- • Catheter material
- • Size and length
- • Number of lumens
- • Insertion site location
- • Dwell time duration
- • Manufacturing defects
Procedural Factors
- • Insertion technique
- • Sterile barrier precautions
- • Multiple insertion attempts
- • Securement adequacy
- • Staff experience level
- • Emergency insertion
Environmental
- • ICU vs. ward setting
- • Staffing levels
- • Workload pressures
- • Protocol adherence
- • Education programs
- • Quality monitoring
4. Evidence-Based Prevention Strategies
PREVENT Mnemonic for IV Complications
Site Selection Optimization
Preferred Sites (Priority Order):
- 1. Cephalic vein (lateral forearm)
- 2. Basilic vein (medial forearm)
- 3. Median cubital vein (antecubital fossa)
- 4. Dorsal hand veins (if necessary)
Avoid: Areas of flexion, infected/inflamed sites, affected limbs (mastectomy, dialysis access), previous IV sites within 24 hours
Catheter Selection Guidelines
Size Selection
- • 24G: Elderly, pediatric, fragile veins
- • 22G: Standard adult peripheral IV
- • 20G: Blood products, viscous fluids
- • 18G: Trauma, surgery, rapid infusions
Material Choice
- • Polyurethane: Flexible, biocompatible
- • Teflon: Smooth, less thrombogenic
- • Avoid: Steel needles for continuous infusion
Length Considerations
- • Short: Reduced infection risk
- • Adequate insertion depth
- • Secure in vessel lumen
5. Sterile Technique Protocols
STERILE Insertion Protocol
2% chlorhexidine in 70% alcohol, 30-second scrub, air dry
Allow antiseptic to completely air dry (minimum 30 seconds)
Gather all supplies, check expiration dates, maintain sterility
Before and after, use alcohol-based hand rub or soap
No-touch technique, bevel up, 15-30° angle
Appropriate dressing, secure without impeding circulation
Confirm blood return, easy flush, no infiltration
Dwell Time Guidelines
Infection Prevention Bundle
- Hand hygiene compliance >95%
- Chlorhexidine skin antisepsis
- Maximal sterile barriers (central lines)
- Daily necessity assessment
- Prompt removal when indicated
6. Monitoring and Assessment Protocols
Assessment Frequency Guidelines
High-Risk Patients
Every 2-4 hours
ICU, immunocompromised, pediatric
Standard Patients
Every 4-8 hours
General medical/surgical units
Ambulatory Patients
Every 8-12 hours
Outpatient/home infusion
Systematic Assessment (STOPS)
Visual assessment for redness, swelling, drainage
Palpate for warmth, coolness, tenderness
Assess flush ability and flow rate
Ask about pain, discomfort, concerns
Check dressing integrity and catheter position
Red Flag Assessment
7. Nursing Implementation Strategies
Clinical Practice Integration
Pre-Insertion Phase
- • Verify physician order and patient consent
- • Assess patient’s IV history and preferences
- • Review allergies and contraindications
- • Select appropriate equipment and location
- • Educate patient about procedure and care
- • Document baseline vascular assessment
Post-Insertion Phase
- • Confirm proper placement and function
- • Apply appropriate securement device
- • Document insertion details and assessment
- • Establish monitoring schedule
- • Educate patient on signs/symptoms to report
- • Plan for timely removal when appropriate
Patient Education
- Signs to watch for and report immediately
- Activity restrictions and arm positioning
- Dressing protection during hygiene
- When to call for nursing assistance
Documentation Requirements
- Insertion site location and appearance
- Catheter type, size, and lot number
- Date, time, and nurse identifier
- Patient response and complications
Quality Improvement
- Track complication rates and trends
- Participate in multidisciplinary rounds
- Contribute to protocol improvements
- Maintain competency through education
Clinical Pearls for Nursing Practice
- • Use ultrasound guidance for difficult access when available
- • Consider topical anesthetic for patient comfort
- • Warm compresses can improve vein visibility and dilation
- • Position patient comfortably to prevent movement during insertion
- • Document failed attempts to guide future insertions
- • Involve vascular access specialists for complex cases
- • Consider alternative access routes early in difficult cases
- • Maintain open communication with patients throughout process
8. Key Memory Aids and Clinical Tips
Phlebitis Scale (Visual Infusion Phlebitis Score)
Action: Grade 2+ requires catheter removal
Infiltration Scale
Action: Any grade requires immediate assessment
Critical Time Points Memory Aid
Key Takeaways for Nursing Practice
Essential Prevention Principles
- • Sterile technique is non-negotiable for all IV procedures
- • Regular assessment prevents minor issues from becoming major complications
- • Early recognition and intervention improve patient outcomes
- • Patient education empowers active participation in care
- • Documentation supports quality improvement initiatives
Clinical Excellence Markers
- • Complication rates <5% in general population
- • First-attempt success rates >80%
- • Hand hygiene compliance >95%
- • Appropriate dwell time adherence >90%
- • Patient satisfaction scores >90%
